Gladstone NOW: The Campaign Join Us on the Journey✕

For World Brain Day, discover some of Gladstone’s latest breakthroughs in neurological research.
From discovering therapies that can repair the brain after stroke to using machine learning to detect early signs of cognitive decline, researchers at Gladstone Institutes are at the forefront of neurological research. Our scientists are not only working to uncover and understand the biological mechanisms behind conditions like Alzheimer’s, Parkinson’s, brain injuries, and more, but are also striving to turn their discoveries into treatments for patients.
On World Brain Day, we’re spotlighting groundbreaking research from Gladstone that expands our understanding of the brain and brings new hope for treating neurological diseases.
Stem Cell Therapy Jumpstarts Brain Recovery After Stroke
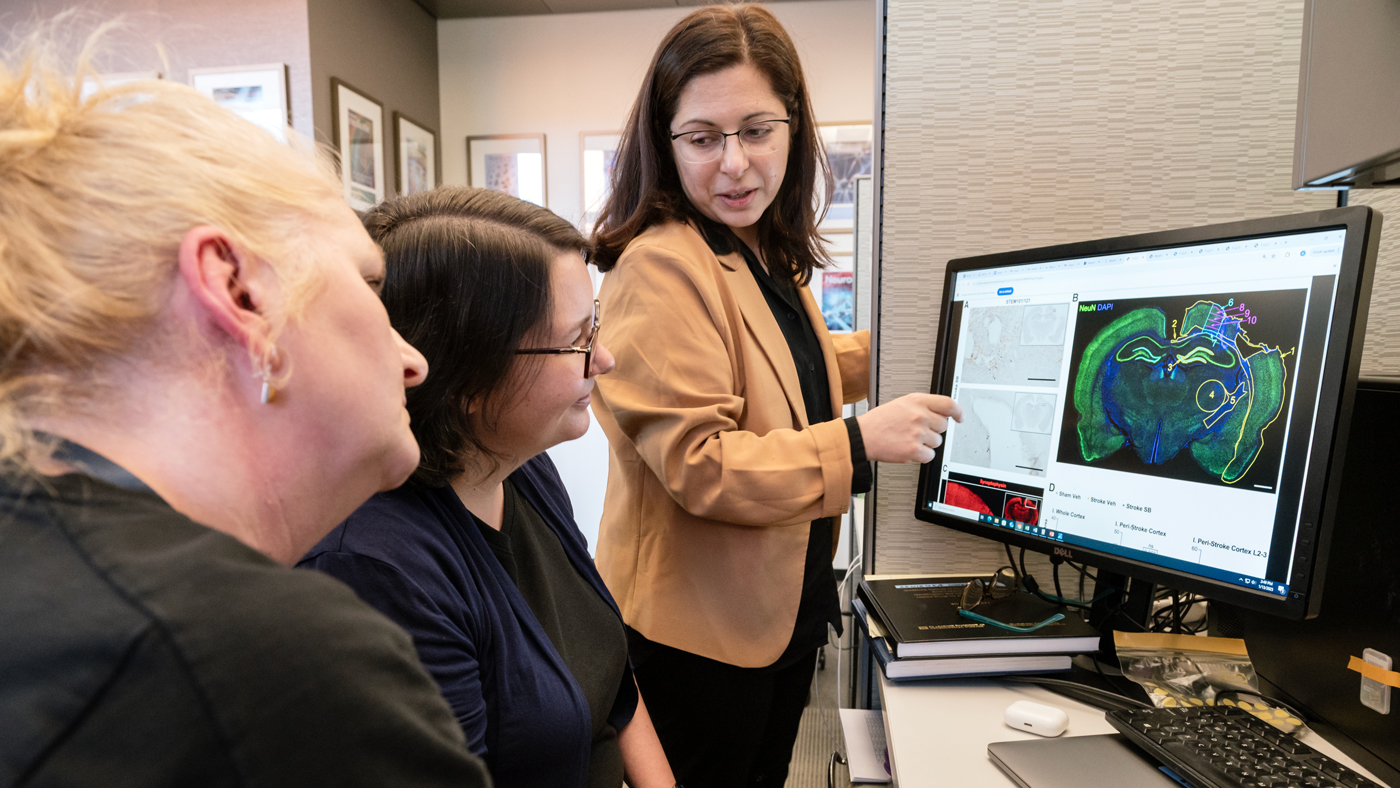
Gladstone researchers, led by Jeanne Paz, PhD, worked with a team at the regenerative medicine company SanBio to show that a cell therapy derived from stem cells can restore normal patterns of brain activity after a stroke. While most stroke treatments must be administered in the immediate hours after a stroke to have a benefit, the study, published in Molecular Therapy, showed the therapy was effective in rats even when given one month later. Read more about the study.
Brain Immune Cells Amplify Damage Caused by Alzheimer’s Risk Gene
A study led by Yadong Huang, MD, PhD, reveals how the APOE4 protein—known as the strongest genetic risk factor for Alzheimer’s disease—interacts with immune cells to drive neurodegeneration. For this study, published in Cell Stem Cell, the researchers used an innovative model in which human neurons producing APOE4 were transplanted into mouse brains. They found that when they removed microglia (immune cells in the brain), the APOE4 protein no longer triggered as many deposits of amyloid or tau—two types of misfolded proteins that are hallmarks of Alzheimer’s disease. This study highlights a promising new target for Alzheimer’s therapies. Read more about the study.
Preventing Brain Damage in Preterm Babies

Visiting Scientist Mark Petersen, MD, worked closely with the lab of Katerina Akassoglou, PhD, to identify a root cause of developmental delays that result from brain bleeds in premature infants, opening a path for new therapeutic strategies to counter long-term health risks. In a study published in Proceedings of the National Academy of Sciences (PNAS), the team showed for the first time that a blood protein called fibrin blocks an essential biological process that drives brain development in early life. Read more about the study.
Machine Learning Reveals Behaviors Linked with Early Alzheimer’s and Points to New Treatments
In a study published in Cell Reports, a team of scientists including Stephanie Miller, PhD, and Jorge Palop, PhD, used a new video-based machine learning tool, called VAME, to pinpoint otherwise-undetectable signs of early disease in mice that were engineered to mimic key aspects of Alzheimer’s. The open-source tool identified subtle behavioral patterns captured on camera—changes that might not be noticed by simply looking at the mice. This work sheds light on a new strategy for identifying neurological disease earlier than currently possible and tracking how it develops over time. Read more about the study.
Discovery of How Blood Clots Harm Brain and Body in COVID-19 Points to New Therapy
A study published in Nature and led by Katerina Akassoglou, PhD, and Warner Greene, MD, PhD, revealed that the blood protein fibrin is not just a byproduct of inflammation in COVID-19, but a primary driver of the disease’s clotting, inflammation, and neurological symptoms. The research shows that fibrin becomes abnormally toxic during infection, binding to the virus and immune cells to form clots that trigger widespread damage and suppress the body’s ability to clear the virus. Importantly, the team also identified a promising antibody therapy that neutralizes fibrin’s harmful effects, offering a potential path to treating both acute and long COVID. Read more about the study.
Powerful New Tool Can Identify Cells Promoting Health or Disease

Stemming from her work on Alzheimer’s disease in the lab of Lennart Mucke, PhD, Cathrine Sant collaborated with Ryan Corces, PhD, to develop a computational tool called CHOIR for distinguishing cells in complex biological samples. The study, published in Nature Genetics, shows that CHOIR outperforms existing methods by accurately identifying biologically meaningful cell types and cell states without generating misleading results, offering a more precise way to uncover cellular drivers of health and disease. Read more about the study.
A New Therapeutic Target for Traumatic Brain Injury
Gladstone scientists, led by Jae Kyu Ryu, PhD, a scientific program leader in the lab of Katerina Akassoglou, revealed that fibrin, a blood coagulation protein, is responsible for initiating toxic inflammation and neuron loss after a major head injury. The findings, published in the Journal of Neuroinflammation, can inform new treatment strategies for a condition that often presents long-term health challenges. Read more about the study.
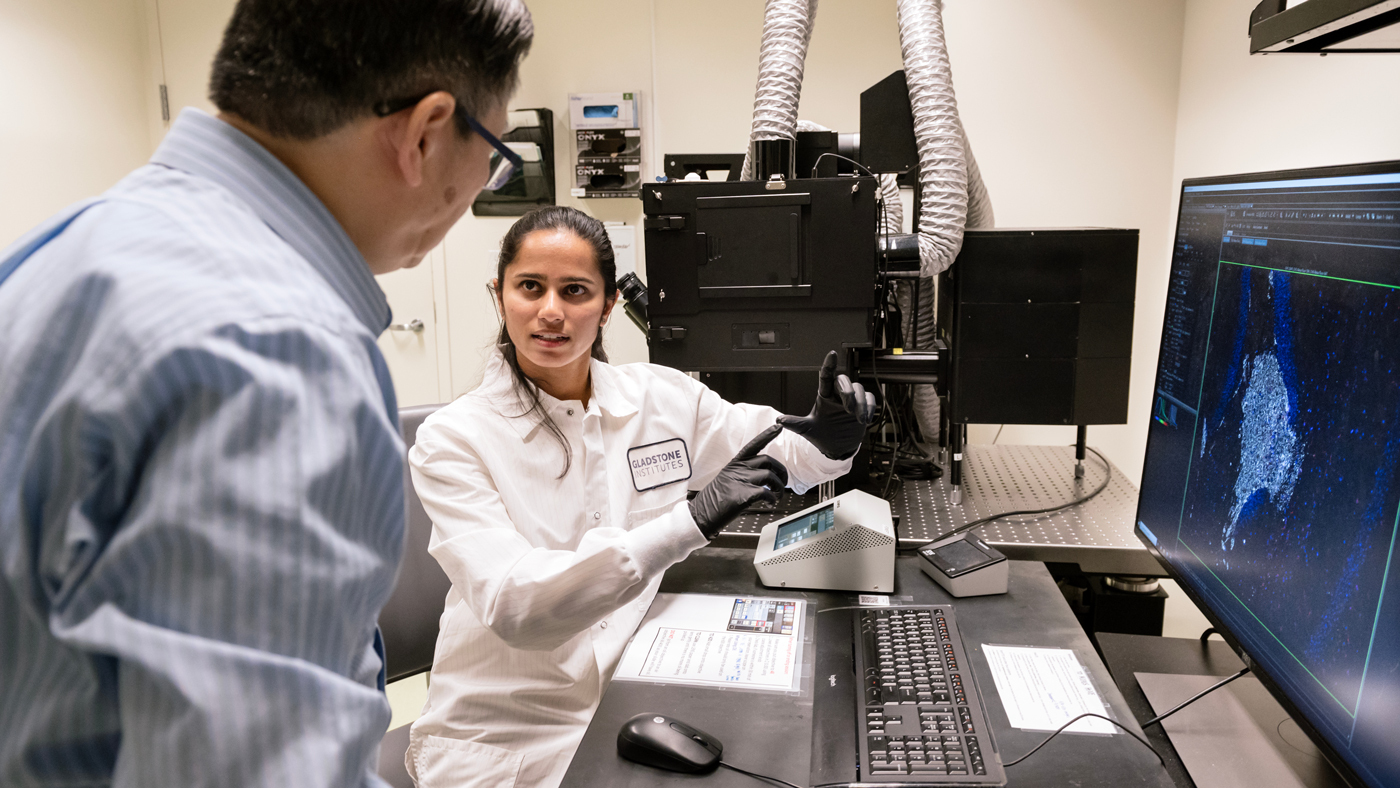
Cellular Clean Energy: Can Mitochondria Make More Energy Without Collateral Damage?
A team at Gladstone led by Ken Nakamura, MD, PhD, used the gene-editing technology CRISPR to investigate within mitochondria exactly which molecules are responsible for creating energy versus those that control the production of reactive oxygen species, or ROS—toxic byproducts commonly known as “free radicals.” Since impaired mitochondria are believed to play a central role in a host of neurodegenerative diseases, the findings, published in Proceedings of the National Academy of Sciences (PNAS), could lead to the development of therapies for diseases such as Parkinson’s or Alzheimer’s. Read more about the study.
Combination of Two Cancer Drugs May Work Against Alzheimer’s
Scientists at Gladstone Institutes and UC San Francisco identified cancer drugs that show promise for reversing changes that occur in the brain during Alzheimer’s disease. In a study published in Cell, Yadong Huang, MD, PhD, and his collaborators used public data to identify gene expressions associated with Alzheimer’s, then looked at data from more than 1,300 drugs that change those gene expression signatures. They found that, when tested in mice, a pairing of two FDA-approved drugs reversed multiple aspects of Alzheimer’s and restored memory. Read more about the study.
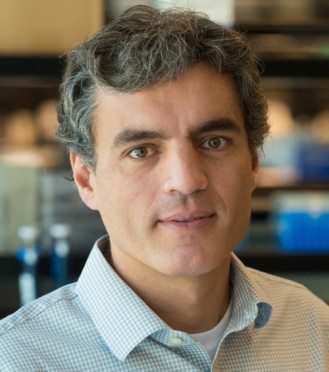
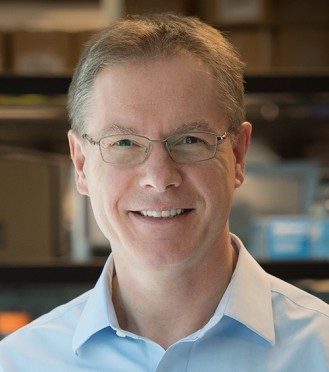
Featured Experts
Gladstone NOW: The Campaign
Join Us On The Journey
Gladstone’s Scientific Highlights of 2025
Gladstone’s Scientific Highlights of 2025
From fundamental insights to translational advances, here’s how Gladstone researchers moved science forward in 2025.
Gladstone Experts Alzheimer’s Disease Autoimmune Diseases COVID-19 Neurological Disease Genomic Immunology Cardiovascular Disease Data Science and Biotechnology Infectious Disease Conklin LabScience in Seconds | Researchers Pinpoint Key Gene Behind Heart Defects in Down Syndrome
Science in Seconds | Researchers Pinpoint Key Gene Behind Heart Defects in Down Syndrome
In this video, Gladstone scientists share how they used stem cells, gene editing, and AI to identify a gene driving heart defects in Down syndrome—and how reducing its levels in mice restored normal heart development, offering hope for future treatments
Gladstone Experts Cardiovascular Disease Data Science and Biotechnology Pollard Lab Srivastava Lab AI Big Data CRISPR/Gene Editing Human Genetics Stem Cells/iPSCsScience in Seconds | The Thinking Microscope: Research Powered by an AI Brain
Science in Seconds | The Thinking Microscope: Research Powered by an AI Brain
In this video, Steve Finkbeiner and Jeremy Linsley showcase Gladstone’s groundbreaking “thinking microscope”—an AI-powered system that can design, conduct, and analyze experiments autonomously to uncover new insights into diseases like Alzheimer’s, Parkinson’s, and ALS.
Gladstone Experts ALS Alzheimer’s Disease Parkinson’s Disease Neurological Disease Finkbeiner Lab AI Big Data