Gladstone NOW: The Campaign Join Us on the Journey✕
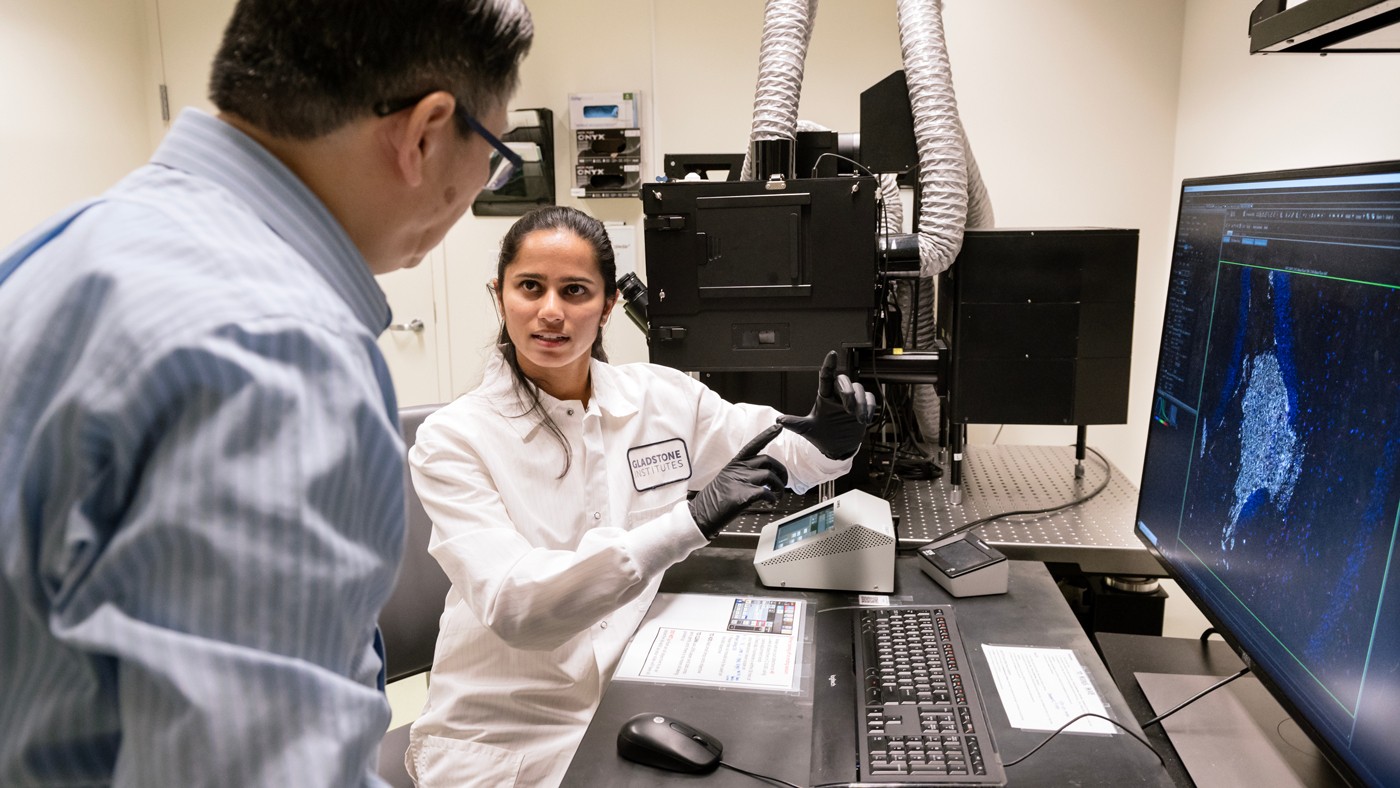
By transplanting human neurons into mouse brains, Yadong Huang (left) and Antara Rao (right) uncovered disease-causing interactions between the APOE4 protein and immune cells called microglia.
In healthy brains, immune cells called microglia patrol for damage, clearing away debris and harmful proteins. But in the presence of the APOE4 protein—the most important genetic risk factor for Alzheimer’s disease—the same cells cause harmful inflammation and clumps of misfolded proteins, according to a new study by scientists at Gladstone Institutes.
The team created a new research model for studying Alzheimer’s that involved transplanting human neurons producing the APOE4 protein into the brains of mice.
When they removed microglia from the brains, they discovered that the APOE4 protein no longer triggered as many deposits of amyloid or tau—two types of misfolded proteins that are hallmarks of Alzheimer’s disease.
“The study underscores the importance of microglia, in concert with APOE4 produced by human neurons, in Alzheimer’s,” says Gladstone Senior Investigator Yadong Huang, MD, PhD, who supervised the new study published in Cell Stem Cell. “Our findings suggest that drugs reducing microglia may eventually be useful in treating the disease.”
A Human-Like Model
There are three major forms of APOE protein in humans. Compared with the most common version of the protein—APOE3—the APOE4 protein increases risk and APOE2 decreases risk for Alzheimer’s disease.
About one in four Americans has at least one copy of the APOE4 gene, and roughly 3 percent have two copies, making those individuals especially susceptible to the disease.
“People with two copies of the APOE4 gene have a 12-fold greater risk of developing Alzheimer’s disease than those with APOE3,” says Huang, who is also director of the Center for Translational Advancement at Gladstone and a professor in the Departments of Neurology and Pathology at UC San Francisco.

Huang (left), Rao (right), and their team created a new mouse model to study how the APOE4 gene contributes to Alzheimer's disease in a much more realistic way than previous models allowed.
To study the complex interplay between APOE variants and brain cells, Huang and his team have long relied on mouse models, just as many other research groups do. However, mimicking the human brain in a mouse is difficult; adding human genes for APOE4 to mice, as is often done, does not fully capture how human brain cells behave in Alzheimer’s disease.
In the new study, Huang’s team developed a “chimeric” mouse model that not only carries human APOE genes, but also contains human neurons that are transplanted into the brain. Importantly, the neurons are transplanted after the brain matures, allowing the researchers to mimic late-onset Alzheimer’s disease.
Previous attempts to establish a mouse model that expresses the characteristics of late-onset Alzheimer’s have been unsuccessful when they used only the APOE4 protein, without transplanted human neurons.
“Creating this mouse model gave us a much more realistic way to study how human neurons carrying the APOE4 gene contribute to Alzheimer’s disease in the living brains of older adults,” says Antara Rao, a graduate student in Huang’s lab who led the experiments for the new study.
Huang and his colleagues already knew that APOE4 leads to higher-than-usual levels of amyloid plaques and tau tangles in human brains. In the new chimeric mouse model, the researchers confirmed that the presence of human APOE4 neurons leads to high levels of both amyloid and tau deposits as the mice aged.
They also showed that human APOE3 neurons lead to moderate levels of the aggregates, and human neurons lacking the APOE gene altogether resulted in fewer tau aggregates and scattered amyloid deposits rather than dense, harmful aggregates.
“It turns out that more accurately modeling late-onset Alzheimer’s disease requires human neurons, rather than mouse neurons, producing APOE4 in mouse brains,” says Huang.
Protective Effect of Reducing Microglia
Huang’s group previously found that mouse neurons producing human APOE4 release molecular signals that activate microglia. This time, they used the new mouse model to probe in more detail the connection between microglia and human neurons producing APOE4.
The researchers used a drug to selectively remove microglia from the brains of the chimeric mice. In mice with human APOE4 neurons, they found that levels of the amyloid and tau aggregates were significantly reduced, indicating that APOE4 and microglia work together to drive key attributes of Alzheimer’s disease.
The study by Rao and her colleagues points to promising strategies for slowing or preventing Alzheimer’s progression in people with the APOE4 gene, who have a greater risk of developing the disease.
The team then turned to single-cell RNA sequencing—a powerful technique to study gene activity in individual cells—to determine what genes were activated in the microglia of each mouse model.
They found that in the presence of human neurons containing APOE4 and APOE3, levels of inflammatory molecules in microglia increased. Microglia with the most inflammatory molecular signatures made up 30 percent of all microglia in mice with human APOE4 neurons, 20 percent of all microglia in mice with human APOE3 neurons, and only 8 percent of all microglia in mice that had human neurons lacking the APOE gene.
“Together, these results suggest that microglia are being activated by human neuron–produced APOE4 and, in turn, are potentially helping form the misfolded protein aggregates we see in Alzheimer’s,” says Rao.
A Path Toward New Treatments
The findings give researchers new inroads to understand how microglia go awry in Alzheimer’s, flipping from its normally protective state to a harmful state in the presence of APOE4 produced by human neurons.
The study also suggests that drugs that can reduce levels of APOE4 in neurons or target microglia—either by reducing the number of microglia or their level of inflammatory activity—could be a promising strategy for slowing or preventing Alzheimer’s disease progression in people with the APOE4 gene.
Still, more work is needed to show whether these potential strategies would be effective in humans, what the side effects of targeting neuronal APOE4 or microglia would be, and how the timing of such treatment would work.
The researchers also hope to use their new chimeric mouse to study the roles of other cell types in Alzheimer’s disease.
“Our new mouse model, along with these initial results, offers a path forward to better understanding Alzheimer’s disease, especially in the context of APOE4, and developing new drugs that could treat it,” says Huang.
For Media
Julie Langelier
Associate Director, Communications
415.734.5000
Email
About the Study
The study, “Microglia Depletion Reduces Human Neuronal APOE4-Related Pathologies in a Chimeric Alzheimer’s Disease Model,” was published in the journal Cell Stem Cell on November 4, 2024. The authors are: Antara Rao, Nuo Chen, Min Joo Kim, Jessica Blumenfeld, Oscar Yip, Zherui Liang, David Shostak, Yanxia Hao, Maxine R. Nelson, Nicole Koutsodendris, Brian Grone, Leo Ding, Seo Yeon Yoon, Patrick Arriola, Misha Zilberter, and Yadong Huang of Gladstone.
The work was supported by the National Institutes of Health (R01AG071697, R01AG076647, 1R01AG065540, P01AG073082, R01AG061150, F31AG074672, F31AG074690), a National Science Foundation Graduate Research Fellowship (2034836), and the Dolby Family.
About Gladstone Institutes
Gladstone Institutes is an independent, nonprofit life science research organization that uses visionary science and technology to overcome disease. Established in 1979, it is located in the epicenter of biomedical and technological innovation, in the Mission Bay neighborhood of San Francisco. Gladstone has created a research model that disrupts how science is done, funds big ideas, and attracts the brightest minds.
Featured Experts
Support Discovery Science
Your gift to Gladstone will allow our researchers to pursue high-quality science, focus on disease, and train the next generation of scientific thought leaders.
New Tool Reveals the Secrets of HIV-Infected Cells
New Tool Reveals the Secrets of HIV-Infected Cells
Developed by Gladstone scientists, HIV-seq could uncover new opportunities for treating HIV.
News Release Research (Publication) HIV/AIDS Infectious Disease Roan LabVitamin B3 Therapy Offers Hope for Fatal Childhood Disease
Vitamin B3 Therapy Offers Hope for Fatal Childhood Disease
A new framework that matches vitamins with genetic diseases helped uncover that high-dose vitamin B3 can dramatically extend survival in mice with NAXD deficiency.
News Release Research (Publication) Rare Diseases Jain LabGladstone Scientist Nadia Roan Elected to American Academy of Microbiology
Gladstone Scientist Nadia Roan Elected to American Academy of Microbiology
Roan has made great strides in understanding how persistent viruses including HIV cause disease and how immunity to viruses shapes human health.
Awards News Release COVID-19 HIV/AIDS Infectious Disease Roan Lab