Gladstone NOW: The Campaign Join Us on the Journey✕
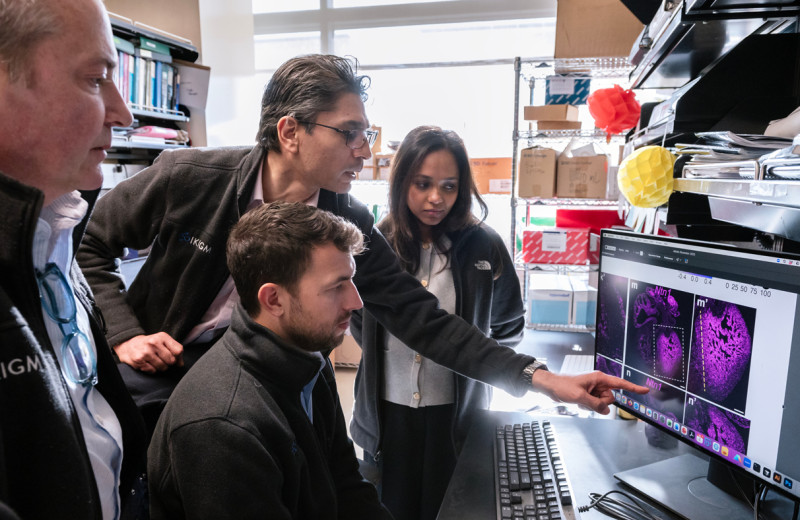
Gladstone staff scientist Neal Bennett (left) and investigator Ken Nakamura are working to solve the question of how to help mitochondria operate more efficiently, which could contribute to new treatment approaches for neurodegeneration and conditions like heart disease, diabetes, and cancer.
Is it possible to amp up the energy production of mitochondria, the “power centers” of cells, without also boosting potentially harmful byproducts? If so, such a method could be used to treat a host of neurodegenerative diseases in which impaired mitochondria are believed to play a central role.
In pursuit of the answer, a team of scientists at Gladstone Institutes used the gene-editing technology CRISPR to parse out exactly which molecules are responsible for creating energy versus those that control the production of reactive oxygen species, or ROS—toxic byproducts commonly known as “free radicals.”
Their findings, which appear in Proceedings of the National Academy of Sciences, could lead to strategies for decoupling energy from ROS production, which may help in the development of therapies for diseases such as Parkinson’s or Alzheimer’s.
“Figuring out how to separate energy production from ROS production is really critical to treating mitochondrial dysfunction,” says Gladstone Investigator Ken Nakamura, MD, PhD, who led the study. “There are many conditions, including neurodegeneration, in which boosting mitochondrial energy could be beneficial, but we don’t want to damage cells through toxic byproducts.”
“There are many conditions, including neurodegeneration, in which boosting mitochondrial energy could be beneficial, but we don’t want to damage cells through toxic byproducts.”
When mitochondria generate cellular energy from sugars and fats, they release ROS. Like pollution spewing from a power plant, ROS have long been considered unwanted but hard-to-prevent byproducts.
Though ROS serve some important biological functions, having too much of them around is toxic to cells and linked with many chronic and degenerative diseases.
Imbalance at the Root of Disease
Solving the question of how to help mitochondria operate more efficiently could contribute to new treatment approaches for neurodegeneration and conditions like heart disease, diabetes, and cancer. It even has implications for healthy aging, as mitochondria become faulty as we grow older.
However, in many cases, it’s tricky to figure out exactly how the mitochondria are malfunctioning: are they not making enough cellular energy, or are they making too much ROS?
Neal Bennett (left), first author of the new study, collaborates with senior author Ken Nakamura. They used CRISPR to determine exactly which molecules are responsible for creating mitochondrial energy versus those that control toxic byproducts commonly known as free radicals.
Nakamura’s group previously screened cells to discover all the genes involved in regulating energy levels. In their new work, they focused on approximately 200 of those genes. Using CRISPR, they worked in cancer cells to selectively turn down the expression of each of those genes and studied what happened to ROS levels.
“We wanted to determine which molecules are required for energy production or ROS production,” says staff scientist Neal Bennett, the first author of the new PNAS study. “By doing that, we were able to discern the genes and pathways that can change those systems independently, which could be very helpful in treating disease.”
Indeed, although some genes affected both energy and ROS production, others had a much stronger effect on one product than the other.
Overall, these findings offer a compelling starting place for researchers who want to develop drugs that independently control mitochondrial energy and ROS and for those trying to understand how mitochondrial dysfunction is implicated in disease.
The team plans to carry out more research on the impact of altered ROS levels on cellular health and to determine whether their results hold true in other cell types, including brain cells.
For Media
Kelly Quigley
Director, Science Communications and Media Relations
415.734.2690
Email
About the Study
The paper “Systems-level analyses dissociate genetic regulators of reactive oxygen species and energy production” was published in the journal PNAS on January 11, 2024. In addition to Ken Nakamura and Neal Bennett, authors include: Megan Lee of Gladstone and Adam Orr, formerly of Gladstone and now with Weill Cornell Medicine.
The work was supported by the National Institutes of Health (R01 AG065428, F32 AG063457, K01AG078485, R01 AGO68091), the UCSF Bakar Aging Research Institute, Aligning Science Across Parkinson's (ASAP-020529) through the Michael J. Fox Foundation for Parkinson’s Research (MJFF), and a Berkelhammer Award for Excellence in Neuroscience.
About Gladstone Institutes
Gladstone Institutes is an independent, nonprofit life science research organization that uses visionary science and technology to overcome disease. Established in 1979, it is located in the epicenter of biomedical and technological innovation, in the Mission Bay neighborhood of San Francisco. Gladstone has created a research model that disrupts how science is done, funds big ideas, and attracts the brightest minds.
Featured Experts
Support Discovery Science
Your gift to Gladstone will allow our researchers to pursue high-quality science, focus on disease, and train the next generation of scientific thought leaders.
Disrupted Boundary Between Cell Types Linked to Common Heart Defects
Disrupted Boundary Between Cell Types Linked to Common Heart Defects
Gladstone scientists identified a cellular boundary that guides heart development and revealed how disrupting it can lead to holes in the heart’s wall.
News Release Research (Publication) Congenital Heart Disease Cardiovascular Disease Bruneau LabGene Editing Strategy Could Treat Hundreds of Inherited Diseases More Effectively
Gene Editing Strategy Could Treat Hundreds of Inherited Diseases More Effectively
Scientists at Gladstone show the new method could treat the majority of patients with Charcot-Marie-Tooth disease.
News Release Research (Publication) Neurological Disease Conklin Lab CRISPR/Gene EditingGenomic Maps Untangle the Complex Roots of Disease
Genomic Maps Untangle the Complex Roots of Disease
Findings of the new study in Nature could streamline scientific discovery and accelerate drug development.
News Release Research (Publication) Marson Lab Genomics Genomic Immunology