Gladstone NOW: The Campaign Join Us on the Journey✕

The 2020 Berkelhammer Scholars break new ground in research on dementias, Parkinson’s disease, and neuropsychiatric disorders. From left to right: Clarissa Mendonça, Zak Doric, Robyn St. Laurent, and Andrew Mendiola.
Brain diseases plague patients across the globe. Neurodegenerative diseases, for instance, already affect millions of people worldwide. And as populations are aging and living longer, the burden of these diseases is rapidly increasing.
To help uncover the causes of these diseases and find better, more effective therapies, four trainees at Gladstone Institutes were selected as the 2020 Berkelhammer Scholars, based on the strength and originality of their research: Robyn St. Laurent, Zak Doric, Andrew Mendiola, and Clarissa Mendonça.
This program, established in 2019, supports high-risk, high-reward research projects on dementia with Lewy bodies and related conditions, such as Alzheimer’s disease, Parkinson’s disease, and neuropsychiatric disorders.
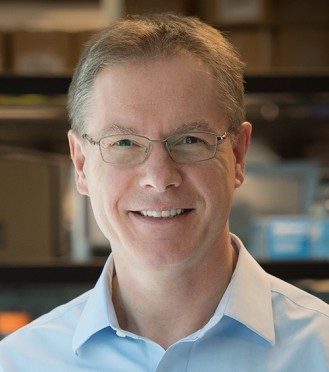
“The program is now enabling a second group of four talented young scientists to pursue an ambitious scientific agenda,” says Lennart Mucke, MD, director of the Gladstone Institute of Neurological Disease. “I believe we are at an inflection point in neuroscience research and the next few years may prove especially critical. I am confident that the trailblazing work of our Berkelhammer Scholars will bring us closer to therapies that previously seemed impossible.”
Addressing the Root Cause of OCD
Robyn St. Laurent, PhD, a postdoctoral scholar in Anatol Kreitzer’s lab, is working to unravel the mechanisms underlying obsessive compulsive disorder (OCD), which is characterized by persistent and intrusive negative thoughts and compulsions, and anxiety surrounding these obsessions.
Although some psychological and pharmacological treatments exist to help patients with OCD, they do not completely alleviate the symptoms, nor do they address the root causes of the disorder.
In part, this is because scientists lack knowledge about the specific brain circuit dysfunctions that occur in OCD, which remains a major hurdle in the development of more effective treatments.
So, St. Laurent’s project focuses on examining OCD-related neural circuits in animal models. By using state-of-the-art techniques, she can temporarily overstimulate cells in different regions of the brain known to regulate fear and anxiety, as a way to determine which circuits elicit responses and behaviors that are similar to OCD.
“This is really where basic research comes in,” says St. Laurent. “By carefully studying these models, my colleagues and I will be able to better understand the connections in the brain that are disrupted in OCD. And that can help us explore more effective therapeutic options.”
Identifying a Culprit of Degeneration in Parkinson’s Disease
Graduate student Zak Doric aims to advance the understanding of Parkinson’s disease, which affects nearly one million Americans and is estimated to cost close to $52 billion per year in the United States alone.
One of the main types of brain cells affected by Parkinson’s disease are neurons that produce a chemical called dopamine. When people lose a subset of dopamine neurons, they develop the motor symptoms that characterize this disease. Other subsets of dopamine neurons, however, seem to be much more resilient.
Doric is trying to figure out why some neurons are particularly vulnerable to Parkinson’s disease. He hypothesizes that the disease causes vulnerable neurons to become hyperactive. Over many years of a person’s life, this hyperactivity places an immense burden on the cells from an energy perspective, which could eventually lead them to decay.
“It remains unknown whether this hyperactivity actually drives degeneration in Parkinson’s, or whether it’s a consequence of the disease,” says Doric, who is part of Ken Nakamura’s lab. “I’m concentrating on this question because no one has been able to answer it.”
With other members of the Nakamura Lab, Doric has developed an animal model to study the hyperactivity of neurons in Parkinson’s disease, allowing him to activate dopamine neurons over a long period of time and recapitulate some of the symptoms seen in patients.
“We can leverage these models to better understand the biological processes in Parkinson’s disease and determine if and how hyperactivity is causing cells to deteriorate,” he says. “If we can identify the major culprits that may be driving cellular degeneration, we can help develop therapies that could be life-changing for millions of people.”
Tackling Alzheimer’s Disease from Different Angles
Two of this year’s Berkelhammer Scholars are taking different, but complementary, approaches to studying Alzheimer’s disease, the most common type of neurodegenerative disorder and the leading cause of dementia.
Clarissa Mendonça, PhD, is studying the greatest genetic risk factor for Alzheimer’s disease, a protein called apoE4. This protein can be found in approximately 25 percent of the population, and in nearly 70 percent of patients with Alzheimer’s disease.
“My greatest motivation for studying this disease is that I know first-hand the drastic impact it can have on people’s lives,” says Mendonça, who is a postdoctoral scholar in the lab of Robert Mahley, Gladstone’s president emeritus who has conducted seminal work on the critical role of apolipoprotein E (apoE). “My grandfather is living with Alzheimer’s right now, and I have lost several close friends to this devastating disease.”
In hopes of one day helping people like her grandfather, Mendonça is trying to understand how apoE4 causes neurodegeneration. By leveraging an approach called proteomics, she can measure thousands of different proteins in neurons and identify the cellular processes that are altered by apoE4.
“My team and I are finding several ways by which apoE4 is impairing the function of neurons that could promote the development of Alzheimer’s disease,” Mendonça says. “Our work could lead to new strategies to treat the disease by preventing the harmful effects of apoE4.”
In parallel to this research on the genetic causes of Alzheimer’s disease, Andrew Mendiola, PhD, a postdoctoral scientist in Katerina Akassoglou’s lab, is investigating how dysfunctions in the brain’s immune system and its interface with the vascular system contribute to neurodegenerative disease.
Akassoglou and her team made the pivotal discovery that when blood leaks into the brain, it elicits a toxic response from the brain’s immune cells, which ultimately leads to neurodegeneration and may promote cognitive decline not only in Alzheimer’s disease, but also in multiple sclerosis and traumatic brain injury.
“No treatments are currently available for slowing or preventing cognitive decline in these disorders,” says Mendiola. “I think a better understanding of the basic mechanisms that are regulating the brain’s immune system may be key for new drug discovery.”
Through his project, Mendiola is trying to identify the unique patterns and triggers that could be driving the toxic immune responses in the brain. To do so, he developed cutting-edge tools to specifically fish out toxic immune cells from the brain in animal models. He can then perform drug screens on the cells to find candidates that can suppress the detrimental immune response and prevent the progression of disease.
“I’m truly honored to be a Berkelhammer Scholar,” says Mendiola. “Thanks to this support of my research, I’m hoping to use the toolbox I’ve developed in other diseases and models of dementia to find new therapeutics that could prevent cognitive decline in patients.”
Featured Experts
Support Discovery Science
Your gift to Gladstone will allow our researchers to pursue high-quality science, focus on disease, and train the next generation of scientific thought leaders.
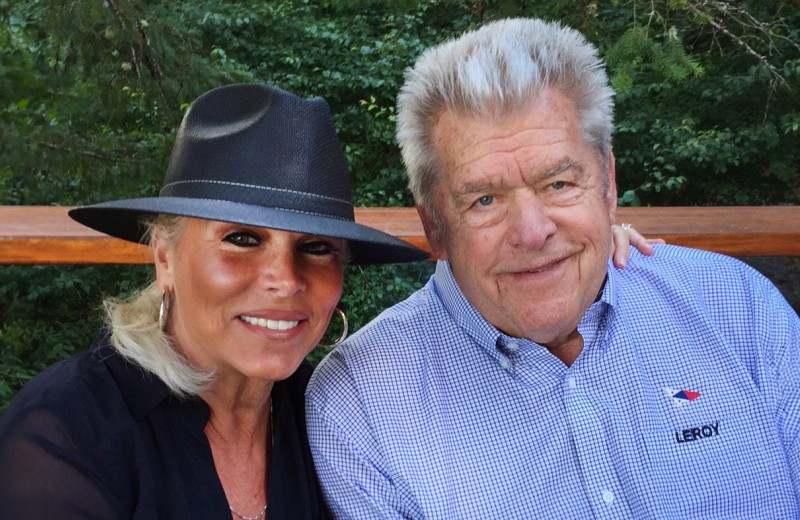
Embracing Change: Darlene Hines Shares Her Journey of Growth, Resilience, and Giving Back
Embracing Change: Darlene Hines Shares Her Journey of Growth, Resilience, and Giving Back
Longtime Gladstone supporter Darlene Hines reflects on her journey of learning, growth, and giving after her husband’s passing
Donor StoriesVisionary Philanthropists Establish Center to Harness Computational Biology for Cancer Research
Visionary Philanthropists Establish Center to Harness Computational Biology for Cancer Research
A search for the brightest minds in cancer and AI led Hope and Sanjit Biswas to give in their own backyard.
Philanthropy Donor Stories Cancer Biswas Center for Transformative Computational Cancer Biology Data Science and Biotechnology Pollard Lab AI Big DataThe Risk and the Reward
The Risk and the Reward
How the Dolby family works to improve outcomes for people with Alzheimer’s disease
Donor Stories Alzheimer’s Disease