Gladstone NOW: The Campaign Join Us on the Journey✕
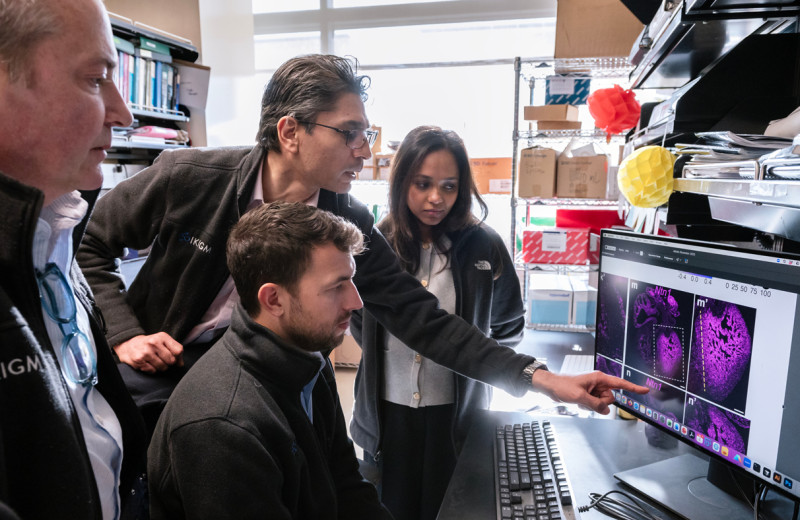
Gladstone Visiting Scientist Nadia Roan and her team found that CD127 cells found in tissues, such as lymph nodes, could be a potential target for an HIV cure.
Scientists have long known that even in the face of antiretroviral therapy, some HIV virus remains in infected individuals forever, hiding in small reservoirs of cells of the immune system. When these individuals discontinue the therapy, the virus almost always rebounds rapidly from the reservoirs, causing deadly symptoms to re-emerge.
These reservoirs remain the main obstacle to curing HIV/AIDS. But there is at present no easy way of targeting reservoir cells for elimination. Nor can scientists efficiently extract reservoir cells from patients to study them, and, ultimately, find ways to control them.
The reason is that the virus in these cells is silent. As a result, the cells do not carry on their surfaces the viral proteins that would make them easy to find.
Scientists have therefore been looking for other means to pinpoint reservoir cells.
In a recent paper in PLOS Pathogens, Gladstone Visiting Scientist Nadia Roan, PhD, and her team describe a class of cells that preferentially support latent infection by HIV. These cells are characterized by a surface protein called CD127 and are found in tissues such as lymph nodes, which are thought to harbor a larger share of the HIV reservoir than blood does.
“Our findings suggest that CD127 cells from tissues may be an important population to target for an HIV cure,” says Roan, who is also an associate professor of urology at UC San Francisco.
In addition, scientists can potentially use the CD127 protein as a handle to isolate reservoir cells from patients, and study what makes them able to silence the virus, and occasionally reactivate it.
A New Reservoir?
HIV targets immune cells, known as T cells, that reside primarily in lymphoid tissues, such as lymph nodes and tonsils. Yet HIV infection studies have largely focused on T cells circulating in the blood, which are relatively easy to gain access to—volunteers are more likely to submit to a blood draw than a tissue biopsy.
But focusing on T cells present in the blood is probably giving scientists a skewed view of the reservoir composition.
“We have long suspected that reservoir cells come in different flavors, and that different tissues harbor different types of reservoir cells. But that has been difficult to show because reservoir cells in infected individuals are rare. The vast majority of in vitro models of latency use cell lines or cells circulating in the blood,” says Roan.
Roan and her team, by contrast, have been studying HIV infection using tissue specimens. In previous work, her team exposed tonsil cells to HIV in the lab to see which ones were most susceptible to infection. Using a variety of experimental approaches, the team found that tonsil cells with the surface protein CD127 efficiently took up the HIV virus but only rarely let it replicate. By contrast, another type of tonsil cells, carrying CD57 on their surface, readily supported a productive infection.
That was intriguing, but that did not necessarily mean that CD127 were reservoir cells.
“After HIV enters a cell, the cell still has ways to escape infection,” says Feng Hsiao, a former research associate in Roan’s lab and co-first author of the present study.
One way is to prevent the virus from copying its genome. Unlike the genome of human cells, the HIV genome is made of RNA. One of the virus’s first tasks upon entering a cell is to make DNA copies of its RNA genome, using a viral enzyme called reverse transcriptase.
Cells can hamper this step by activating an enzyme called SAMHD1 that depletes the stores of building blocks the virus needs to copy its genome. There was some evidence that this mechanism might be at play in blood cells.
However, in their present work, Roan and her team found that eliminating SAMHD1 by genetic manipulation did not allow CD127 cells to churn out virus, even though it boosted viral production by CD57 cells.
“This suggested to us that CD127 cells blocked the virus at a later step in its life cycle,” says Julie Frouard, PhD, a postdoctoral scholar in Roan’s lab and the other first-author of the study.
A Preference for Latent Infection
The next step for the virus is to integrate a copy of its genome into the host cell’s DNA. Once there, the viral genes can take advantage of the cell machinery to produce their own proteins, which assemble new viral particles that can go infect other cells.
Reservoir cells harbor HIV’s genetic material integrated in their own genomes, though they somehow silence it. The occasional mobilization of this material permits the release of infectious virus. Did CD127 tonsil cells allow HIV genome integration?
“Ultimately, our hope is that the mechanisms we uncover can be harnessed to control the latent reservoir and move us closer to achieving a cure for HIV”
To answer this question, the scientists extracted the genome of CD127 and CD57 cells that had been exposed to virus in the lab. Using genetic tools that can specifically detect integrated viral DNA sequences, they found that both cell types harbored copies of the virus’s genome, even though CD127 cells produced far less virus than CD57 cells did. The CD127 cells appeared to favor a latent infection.
And yet, the virus integrated in CD127 cells is not silenced forever. Roan and her team found that by treating latently infected CD127 cells with agents known to stimulate T cells, they could coax the cells to reactivate the virus.
Hence, CD127 tissue cells could very well serve as reservoir cells in the body, keeping the virus dormant most of the time, yet able to occasionally activate it and release the seeds of a new round of infection.
“The ability of a specific type of tissue T cell to preferentially support latent infection is very intriguing, and can teach us much about how the tissue reservoir becomes established initially,” says Roan.
Controlling the Reservoir
To what extent CD127 cells are a major component of the reservoir in people living with HIV awaits follow-up studies analyzing these cells from multiple tissue sites. Preliminary studies from Roan’s team are encouraging, as they show that the CD127 marker on the cells’ surface can indeed be used to purify enough infected tissue cells from infected individuals to allow further analyses.
Meanwhile, “CD127 tonsil cells exposed to HIV in vitro provide a novel model to study viral latency in tissues,” says Roan.
Roan and her team have already started analyzing what makes CD127 cells uniquely prone to silent infections. By comparing all the genes expressed in CD127 and CD57 tonsil cells, they found evidence that CD127 cells are in a quiescent state that may prevent the expression of the virus’s genes. Moreover, they also found that the virus’s gene products, or RNAs, failed to undergo the necessary processing that would allow them to make viral proteins.
“Ultimately, our hope is that the mechanisms we uncover can be harnessed to control the latent reservoir and move us closer to achieving a cure for HIV,” says Roan.
For Media
Julie Langelier
Associate Director, Communications
415.734.5000
Email
About Gladstone Institutes
Gladstone Institutes is an independent, nonprofit life science research organization that uses visionary science and technology to overcome disease. Established in 1979, it is located in the epicenter of biomedical and technological innovation, in the Mission Bay neighborhood of San Francisco. Gladstone has created a research model that disrupts how science is done, funds big ideas, and attracts the brightest minds.
Support Discovery Science
Your gift to Gladstone will allow our researchers to pursue high-quality science, focus on disease, and train the next generation of scientific thought leaders.
Disrupted Boundary Between Cell Types Linked to Common Heart Defects
Disrupted Boundary Between Cell Types Linked to Common Heart Defects
Gladstone scientists identified a cellular boundary that guides heart development and revealed how disrupting it can lead to holes in the heart’s wall.
News Release Research (Publication) Congenital Heart Disease Cardiovascular Disease Bruneau LabGene Editing Strategy Could Treat Hundreds of Inherited Diseases More Effectively
Gene Editing Strategy Could Treat Hundreds of Inherited Diseases More Effectively
Scientists at Gladstone show the new method could treat the majority of patients with Charcot-Marie-Tooth disease.
News Release Research (Publication) Neurological Disease Conklin Lab CRISPR/Gene EditingGenomic Maps Untangle the Complex Roots of Disease
Genomic Maps Untangle the Complex Roots of Disease
Findings of the new study in Nature could streamline scientific discovery and accelerate drug development.
News Release Research (Publication) Marson Lab Genomics Genomic Immunology