Gladstone NOW: The Campaign Join Us on the Journey✕

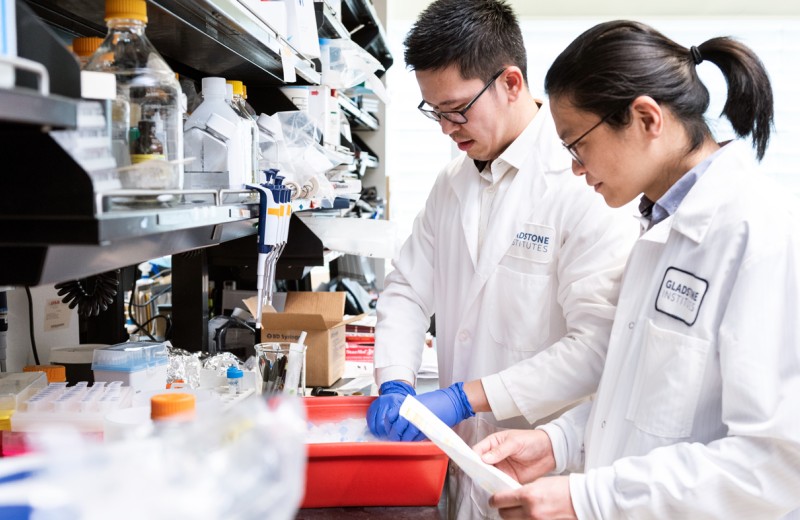
Dr. Jeanne Paz is using light to stop seizures. Her groundbreaking work may transform epilepsy research and lead to better treatments. [Photo: Chris Goodfellow]
Epilepsy, and the seizures that accompany it, can have a genetic origin or may occur following a brain injury or stroke. Whatever the cause, seizures affect 50 million people worldwide, and an alarming 15 million of these individuals lack effective treatment for their condition. Moreover, many available therapies have debilitating side effects that prevent patients from leading normal lives.
Using Light to Quiet a Seizure
Jeanne Paz, PhD, an assistant investigator at the Gladstone Institutes, is trying to change this difficult reality. In a groundbreaking study published in Nature Neuroscience, Dr. Paz used a powerful research tool called optogenetics to stop a seizure as soon as it begins, opening the door for alternative therapies.
With optogenetics, scientists can turn specially modified cells in the brain on or off just by shining a light in the region. While this technique is currently only available in animal models, it provides an important window into the brain generally—revealing the roles different cells play and identifying potential new targets for drug treatments in humans.
In the epilepsy study, Dr. Paz used optogenetics in a mouse model to silence the hyperactive brain cells that cause seizures, cutting the attacks short. To do so, she used an electroencephalograph (EEG) to detect a seizure as soon as it began. The EEG then triggered a light to turn on in the mouse’s brain, immediately blocking the cells’ abnormal activity.
“This was the first demonstration that we could stop a seizure in real time,” says Dr. Paz. “By interrupting a seizure at the time of its onset, we can prevent it from developing and spreading to other parts of the brain.”
Targeting Choke Points in the Brain
Dr. Paz used another unique approach in her study. Instead of focusing on the part of the cortex where the seizure started, she treated cells downstream in an area called the thalamus. The thalamus acts as a kind of relay station in the brain, receiving input from the cortex and projecting signals back out to different regions. Dr. Paz thinks that the thalamus may serve as a “choke point” for cortical seizures and targeting this area can halt abnormal brain activity before it spreads further.
“The start of a seizure is incredibly quick and nearly impossible to catch,” explains Dr. Paz. “But from there it engages a large-scale network, and lots of different brain areas become involved. So instead of focusing on the origin of the seizure, which we might not identify in time, we propose going after a strategic point in the network—a choke point that can cut off the abnormal activity.”
Currently, Dr. Paz is testing this method in cortical epilepsies that result from a traumatic brain injury or stroke. However, she hopes that the choke point theory will also prove beneficial in epilepsies that originate in different areas of the brain, like temporal lobe epilepsy, which is more likely to have a genetic cause. The next step is to find choke points for other types of seizure disorders and see if they have the same powerful effect.
While it might seem counter-intuitive to treat a healthy part of the brain, Dr. Paz says that with optogenetics the brain is only affected when a seizure is happening. This reduces any possible side effects from the treatment. In contrast, seizure medications have both a chronic and global impact on brain function, affecting nearly all areas of the brain all of the time. This can result in unpleasant side effects, such as lethargy, dizziness, and difficulty concentrating.
“The beauty of optogenetics is that there is no negative impact on normal brain activity,” says Dr. Paz. “In our mouse model, the therapy did not affect behaviors such as eating, sleeping, or movement in any way.”
Translating Basic Research into Treatments
Although optogenetics is not yet possible in humans, Dr. Paz believes we may be able to use similar therapies like deep brain stimulation to target a specific area in real time to stop a seizure. Additionally, the insights gained from this research may also help scientists develop new drugs that are more selective to a particular region or type of brain cell.
“Studies using optogenetics have the capacity to make an enormous impact on translational research,” she says. “Better epilepsy treatments will improve the quality of life for millions of people.”
Want to Join the Team?
Our people are our most important asset. We offer a wide array of career opportunities both in our administrative offices and in our labs.
Explore CareersMeet Gladstone: Britta Lindquist
Meet Gladstone: Britta Lindquist
In honor of National Epilepsy Awareness Month, Postdoctoral Scholar Britta Lindquist shares how her past experiences in medical school brought her to study epilepsy.
Graduate Students and Postdocs Epilepsy Paz LabZeroing in on a New Treatment for Autism and Epilepsy
Zeroing in on a New Treatment for Autism and Epilepsy
Gladstone scientists show that reducing levels of the protein tau soon after birth can prevent these conditions in an experimental model
News Release Research (Publication) Epilepsy Neurological Disease Mucke LabMaintaining Balance in the Brain
Maintaining Balance in the Brain
Gladstone scientists help explain how reducing the protein tau can prevent abnormal brain activity associated with Alzheimer’s disease, autism, and epilepsy
News Release Research (Publication) Alzheimer’s Disease Epilepsy Neurological Disease Mucke Lab