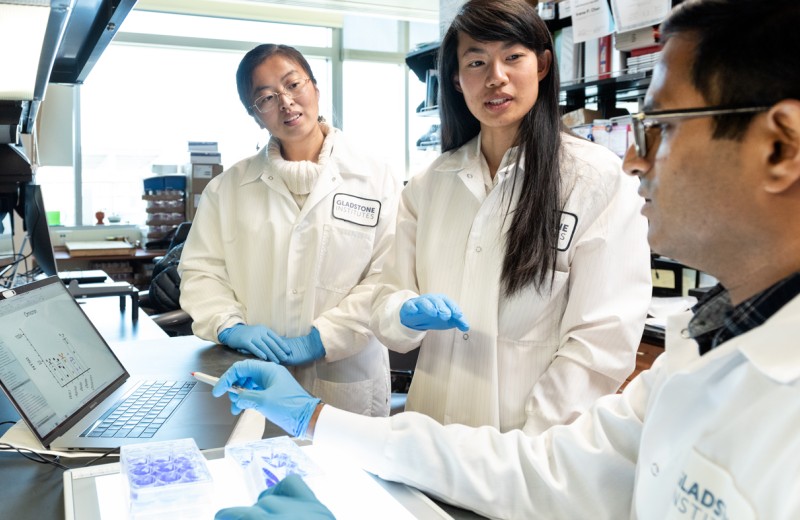
In response to the COVID-19 pandemic, many Gladstone scientists have rapidly pivoted the focus of their research labs to the novel virus, SARS-CoV-2. Specifically, they are leveraging their established tools, unique infrastructure, and diverse expertise in virology to develop improved diagnostics, identify targeted treatment strategies, and invent preventative approaches.
Gladstone scientists were instrumental in converting HIV/AIDS from a uniformly lethal disease into a chronic condition, and are now bringing the same urgency and focus to combatting COVID-19 in a comprehensive manner.
Image Credit: Novel Coronavirus SARS-CoV-2 by NIAID is licensed under CC BY 2.0
How Gladstone Is Contributing
Diagnostics
Gladstone scientists are collaborating to develop a CRISPR-based method to rapidly measure COVID-19 RNA. By combining the technique with smartphone technology, they aim to develop a diagnostic that could deliver rapid results and be widely deployed even far from traditional labs, such as in airports and other ports of entry, and in remote communities throughout the world. Another team is applying machine learning to discover biomarkers that will predict which patients are most likely to experience severe disease, and which may have an asymptomatic course.
Treatment
Gladstone researchers mapped interactions between human host cell proteins and the virus, and are now using this information to identify therapeutic targets. Others are screening libraries of FDA-approved drugs and testing their effects on the virus in human lung “organoids” and human heart cells. Additional projects include investigating how the virus affects the brain, leading to cerebrovascular complications and stroke, and studying ways to rejuvenate the immune system to improve its ability to fight infection.
Prevention
A Gladstone team is investigating the potential of an innovative alternative to a vaccine. Therapeutic interfering particles (TIPs) could turn the tables on the virus by hijacking its machinery to transform virus-infected cells into factories that produce more therapeutic particles than virus, slowing its spread.
Current Research Projects
How Long COVID Affects our Immune Systems
It is estimated that approximately 10% of people who get COVID-19 develop lingering health problems, referred to as Long COVID. Nadia Roan, PhD, and her lab are focusing on improving our understanding of Long COVID and identifying novel and effective treatments for it.
In a recently completed study, the Roan Lab collaborated with clinicians at UC San Francisco to compare immune cells and proteins between those with and those without Long COVID 8 months after recovery from COVID-19. They applied state-of-the-art technologies and focused on analyzing T cells, important fighters against viral infections that can also potentially go rogue when dysregulated. The scientists found that there were sex-dependent differences in T cells associated with Long COVID, and that those with Long COVID had mis-migrating and “exhausted” T cells that were dis-coordinated between the antibody and T cell arms of immunity. The next step is to expand this study, analyzing whether similar immune dysregulation occurs in tissues where the persistence of SARS-CoV-2 may drive Long COVID symptoms. This will improve scientists’ understanding of the mechanistic basis of Long COVID in order to design targeted therapies for the condition.
Finding a Model for Long COVID
In a second Long COVID study, Nadia Roan, PhD, and her team collaborated with other Gladstone scientists – Melanie Ott, MD, PhD, and Jorge Palop, PhD. Currently, there isn’t an appropriate animal model of Long COVID. One key reason for this is that there is no one test or symptom that defines Long COVID in humans; diagnosis is based on an extensive list of questionnaires. To address this urgent need, the scientists applied new technologies from the neurobiology field that deploy AI to analyze mouse behavior. While originally developed to study neurodegenerative diseases, this technology was essential in order to identify subtle disease-associated abnormalities. Applying these same approaches to mice that had recovered from mild COVID-19, they found evidence of cognitive abnormalities, including behaviors reminiscent of “brain fog.” They then performed state-of-the-art immunological studies on the mice’s cells and found multiple abnormalities compared to mice that were never exposed to COVID-19.
Strikingly, they found that a specific protein called CXCR4 that was previously implicated in severe COVID-19 and Long COVID in humans was present at high levels in the Long COVID mice but not the control mice. Drugs targeting this protein have shown beneficial effects when tested in models of CXCR4-driven asthma. The scientists aim to test this and related inhibitors in the new Long COVID mouse model. They also aim to expand the model in the context of risk factors for Long COVID, such as diabetes and other comorbidities.
CRISPR Diagnostic
Melanie Ott, MD, PhD, Jennifer Doudna, PhD, and Katie Pollard, PhD, have collaborated with others at UC Berkeley and the Innovative Genomics Institute to develop a portable, low-cost, CRISPR-based COVID-19 diagnostic test. This novel test combines the accuracy of a PCR test with the low cost, portability, and simplicity of an antigen test. Not only can the test detect whether a sample is positive for the COVID-19 virus, it can also determine how much virus is in a sample. Gladstone scientists are working with industry partners to do the final validation tests required before launching the test on a larger scale.
Currently, the team is working on multiplexing the technology so that the test can detect and discern between COVID-19, influenza A, B, and RSV A, B in a single sample.
Faster Ways to Model New Variants
It is important to be able to generate the full length of the SARS-CoV-2 virus’s genetic material synthetically in a lab, as there are often delays in obtaining patient isolates and risks associated with mutations that can arise when viruses are propagated for a long time in a lab. The SARS-CoV-2 genetic material in particular, is quite long, adding to the challenge.
Taha Taha, PharmD, PhD, in collaboration with Melanie Ott, MD, PhD, Jennifer Doudna, PhD, and others developed a strategy to generate noninfectious replicating particles of a virus within a week. These particles don’t have structural proteins such as spike and so cannot spread. They can, however, replicate viral RNA for study. The scientists used this method to construct several naturally occurring versions of the virus and discovered what made the omicron variant less severe. This technology is also being used for many other projects in the lab to uncover the mechanisms of SARS-CoV-2 pathogenesis. One promising study is looking for new antiviral strategies against a specific target protein and another one is testing hundreds of mutations simultaneously to identify the next variant of concern.
Mapping New Drug Targets
Nevan Krogan, PhD, and his team are studying the points of interaction between SARS-CoV-2 and our cells to find new drugs to stop the virus. They examine the viral genome as well as 10 additional viral proteins that are needed to create more of the virus, evade the human immune system, and other roles. Using cutting-edge tools developed by the Krogan Lab, the scientists are studying the physical structure of viral proteins and the human proteins they interact with to learn where on the proteins potential drugs will most likely be able to stick and interfere with essential viral processes. The team then designs and tests large numbers of potential drugs to determine if they can prevent the virus from spreading.
Since the pandemic began, Krogan and his team have identified all of the human proteins that interact with the virus and identified 66 druggable human proteins targeted by 69 compounds, of which 29 drugs are already FDA-approved, 12 are in clinical trials, and 29 are preclinical compounds. One of the drugs identified through this approach was more effective than remdesivir in testing and is currently in clinical trials.
Recently, the team has been working to understand how some variants are more transmissible or escape the human immune system, how the virus changed when it jumped from animals to humans, and using a systems biology approach to develop new drugs less susceptible to viral resistance.
Modeling Lung Function
The Ott Lab has developed human lung organoids to serve as accurate and analogous models of human lungs to study how COVID-19 affects our airways. Using these organoids, scientists have studied whether infection with the omicron variant of COVID-19, which has milder symptoms, could lead to protection from future variants. This is important to study as new variants emerge—especially as it relates to immunity derived from vaccination.
In collaboration with Nadia Roan, PhD, Jennifer Doudna, PhD, and UC San Francisco scientists, they found that infection with omicron can increase pre-existing immunity in vaccinated, but not unvaccinated, individuals. This finding is informing strategies for multivalent vaccines and boosters utilizing antigens from multiple circulating variants.
A New Treatment Strategy
Leor Weinberger, PhD, has developed a novel strategy to treat and even prevent COVID-19. His team has engineered molecules called therapeutic interfering particles (TIPs) that turn the virus against itself.
Originally developed as a strategy to treat HIV, TIPs are defective forms of the virus that are able to replicate and spread among cells, but do not cause disease. They evolve and spread alongside the virus, outcompeting it for cellular resources. Ultimately, the innocuous TIPs could block the SARS-CoV-2 virus from making us sick and eliminate the need for vaccine and booster shots. The team has shown that a single administration of COVID-19 TIPs was effective in suppressing the virus and preventing transmission in hamsters. This work has been validated in large-scale animal studies and the team is now moving the treatment toward a clinical trial.
Stopping Viral Spread
Warner Greene, MD, PhD, and collaborators have developed a new strategy to prevent transmission of SARS-CoV-2. The scientists have discovered a peptide, a short string of amino acids similar to but smaller than a protein, that targets the spike protein and blocks the viral fusion necessary for the virus to enter our cells. They have developed an intranasal preventive spray and have launched a company to bring this novel preventive treatment to the public.
Implications for the Heart
While COVID-19 is primarily a respiratory disease, it can also cause heart damage that lingers even after recovery. Gladstone scientists Bruce Conklin, MD, and Todd McDevitt, PhD, studied how COVID-19 damages the heart on a cellular level.
They found that the virus infects and kills the heart’s muscle cells, which are necessary for the contraction and relaxation involved in heartbeats. They also discovered that sarcomeres, the contractile units of heart muscle, are sliced up into smaller fragments by the virus. Strikingly, this damage was observed irrespective of disease severity, such that even patients with mild disease might suffer lasting heart damage.
COVID-19 in the Brain
The Greene Lab used human brain organoids to study how COVID-19 causes neural damage. They learned that the primary cellular targets for the virus in the brain are specialized brain cells called astrocytes. These cells have a different receptor that mediates SARS-CoV-2 infection – Neuropilin-1 rather than ACE2. The scientists tested variants of concern and how they made use of this alternative viral receptor. Their findings suggested that the most highly infectious variants may display different effects within different tissues due to receptor specificity tradeoffs.
Lab Upgrades
In 2020, Gladstone brought a dedicated biosafety lab online to meet the high containment standards necessary to study SARS-CoV-2, the virus that causes COVID-19. We swiftly upgraded the air filtration system, installed new lab equipment, implemented new processes to safely operate in the lab, and provided specialized training for lab personnel. We also procured appropriate personal protective equipment required for this type of lab amid a global shortage. The facility houses a 100-cage capacity for mice and a 16-cage capacity for hamsters and is ideal for airborne transmission studies and a wide variety of instruments to perform complex experiments and procedures using risk group 3 agents in a regulated and safe environment.
Virology Experts

Senior Investigator, Gladstone Institutes

Senior Investigator, Gladstone Institutes

Senior Investigator, Gladstone Institutes
Research Integrity Advisor; Chair, Conflict of Interest Committee

Senior Investigator, Gladstone Institutes
Director, Gladstone-UCSF Institute of Genomic Immunology

Director, Gladstone Institute of Virology

Director, Gladstone Institute of Data Science and Biotechnology

Senior Investigator, Gladstone Institutes
Support Our COVID-19 Research Efforts
Gladstone scientists are moving quickly to respond to the coronavirus outbreak. Help us end this pandemic.
Donate NowFAQs
How Does the Coronavirus Spread?
Coronaviruses are a large family of viruses that predominantly circulate in bats. They occasionally transmit from bats to other animals, and then to people. The virus responsible for the current outbreak, now called SARS-CoV-2, is thought to primarily spread from person-to-person through respiratory droplets, which are created when a person coughs or sneezes.
What Are the Symptoms of Infection, and When Should People Seek Medical Advice?
The most common symptoms are fever, cough, and shortness of breath. If you experience these symptoms, contact your health care provider to schedule a COVID-19 test. Most people will recover on their own by keeping their fever under control, using a room humidifier, staying well-hydrated, and basically staying home to rest. If symptoms become worse or concerning, call your health care provider to seek additional care. Many people elect to monitor their oxygen saturation using a pulse-oximeter
How Does the Vaccine Work?
In the United States, there are currently two approved COVID-19 vaccines, one from Moderna, and one from Pfizer/BioNTech. Both of these vaccines use the viral genetic code to induce an immune reaction that teaches your body to recognize and fight SARS-CoV-2 the next time you encounter it. Neither of these vaccines introduce live virus into your body, so vaccination cannot give you COVID-19. These vaccines require two shots for full efficacy, which are given a few weeks apart.
Additional very promising vaccine candidates are awaiting FDA authorization, and may be available soon. The more people who are vaccinated against COVID-19, the more slowly the disease will spread, and the safer our communities will be.
How Does Testing Work and Who Can Administer the Test?
The most common test, the PCR test, looks for presence of the virus itself. It is based on nasal swabs or pharyngeal (throat) swabs, or can in some cases be done from saliva. San Francisco and many other municipalities provide free testing sites you can visit if you have been in contact with someone who is infected, or if you are experiencing symptoms. You can also contact your healthcare provider to schedule a test.
Are There Extra Precautions One Should Take If Pregnant?
As far as we know today, there is no known risk to the fetus if the mother is affected with COVID-19, at least in the late stages of the pregnancy, so this is very different from other illnesses like the Zika virus infection. But it is clear that pregnant women have a somewhat weakened immune system, so if you are pregnant, you are generally more susceptible to infection (by any virus), and extra precautions should be taken. You should practice social distancing, and all the hygiene recommendations that are in place should be taken very seriously. Find out more about higher-risk populations.
Are the New Coronavirus Variants More Dangerous?
Viruses mutate frequently, and several SARS-CoV-2 variants are currently circulating around the world. There is some evidence that these variants can spread more quickly through populations, but it is not yet clear whether they cause more severe disease. It is possible that the neutralizing antibodies generated by the currently available vaccines may be somewhat less effective against particular variants (those found in South Africa and Brazil), although the vaccines should continue to protect against severe infection and hospitalization.
“Gladstone is perfectly positioned to respond to the current coronavirus pandemic. Our scientists are working together to pivot their research to address this major public health crisis.”
Are You a Journalist?
As coronavirus concerns grow, Gladstone’s experts are here to answer your questions, offer insight, provide context, and discuss the impacts of the outbreak on public health.
Talk to an Expert