Gladstone NOW: The Campaign Join Us on the Journey✕
Gladstone scientists—including Juan Perez-Bermejo (seen here on the right)—revealed that a variant of the BAG3 gene could have protective effects in people with a predisposition for heart disease.
For years, a gene known as BAG3 has intrigued heart researchers around the world. That’s because genetic studies suggest that nearly 1 billion people have a version of the BAG3 gene that is associated with a lower risk of heart failure.
However, it has been unclear whether this “good” version—known as BAG3C151R—directly protects the heart in a meaningful way, or if the association is merely incidental, with little clinical relevance.
Now, after 10 years of painstaking work, researchers at Gladstone Institutes have revealed that BAG3C151R has specific molecular interactions that could lead to a protective effect for people who carry this variant. They also showed that the variant is sufficient to provide protection from heart failure to heart cells in a dish. This discovery sets the stage for the development of novel treatments to reduce people’s risk of heart failure.
The new work was published in the journal Nature Cardiovascular Research and led by Gladstone Senior Investigator Bruce Conklin, MD, and Juan Perez-Bermejo, PhD, a former postdoctoral scholar in his lab.
We asked Conklin and Perez-Bermejo to share more about the research.
What Makes this Version of BAG3 So Intriguing?
Perez-Bermejo: The BAG3 gene makes a protein that, in essence, performs “quality control” to ensure the proper function of other proteins that maintain good heart health—especially when heart cells are under stress. We’ve known for many years that people with certain very rare DNA mutations in BAG3 have weakened heart muscles, which can lead to heart failure.
At the same time, many large genetic studies have linked another version of this gene, called BAG3C151R, to lower risk of heart failure. And this one isn’t as rare: about 20 percent of people of European and Southeast Asian descent have it.
But it’s one thing to see a link between this version of the gene at the population level and lower risk of heart failure, and a whole different, far more challenging task to validate whether it is biologically meaningful. It’s possible that it could just be an association—perhaps intermingled with race or country, cultural or lifestyle factors, or even other genes—and that the gene might not actually play an important role in heart health.
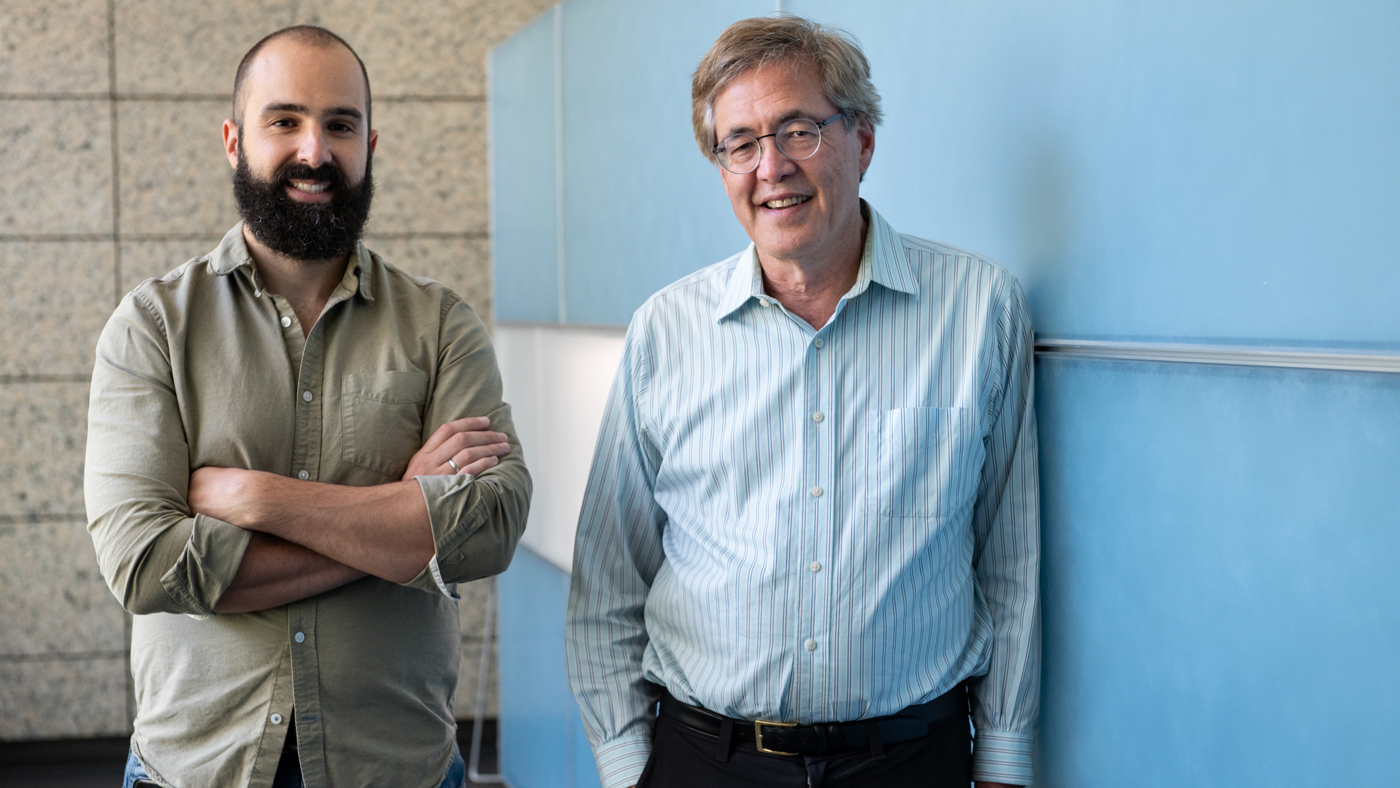
Perez-Bermejo (left) and Conklin (right) found strong evidence that BAG3C151R may directly contribute to a lower risk of heart failure in people.
Why Is It Challenging to Validate the Biology behind This Kind of Association?
Conklin: A DNA change associated with a lower risk of a certain disease in a large population is very difficult to follow up on because a protected person may simply seem unremarkably healthy. It’s pretty much impossible to tell exactly why the person does not have the disease. It’s much more straightforward to show what does cause disease. So, typically, researchers focus on disease-causing mutations that have the same detectable consequences for every person with the mutation.
That extends to the lab, where it can be relatively easy to see the effects of a disease-causing mutation in a cell in a dish, but far more difficult to determine exactly why a healthy cell is healthy. That’s a major reason why researchers almost never follow up on protective associations seen in population studies.
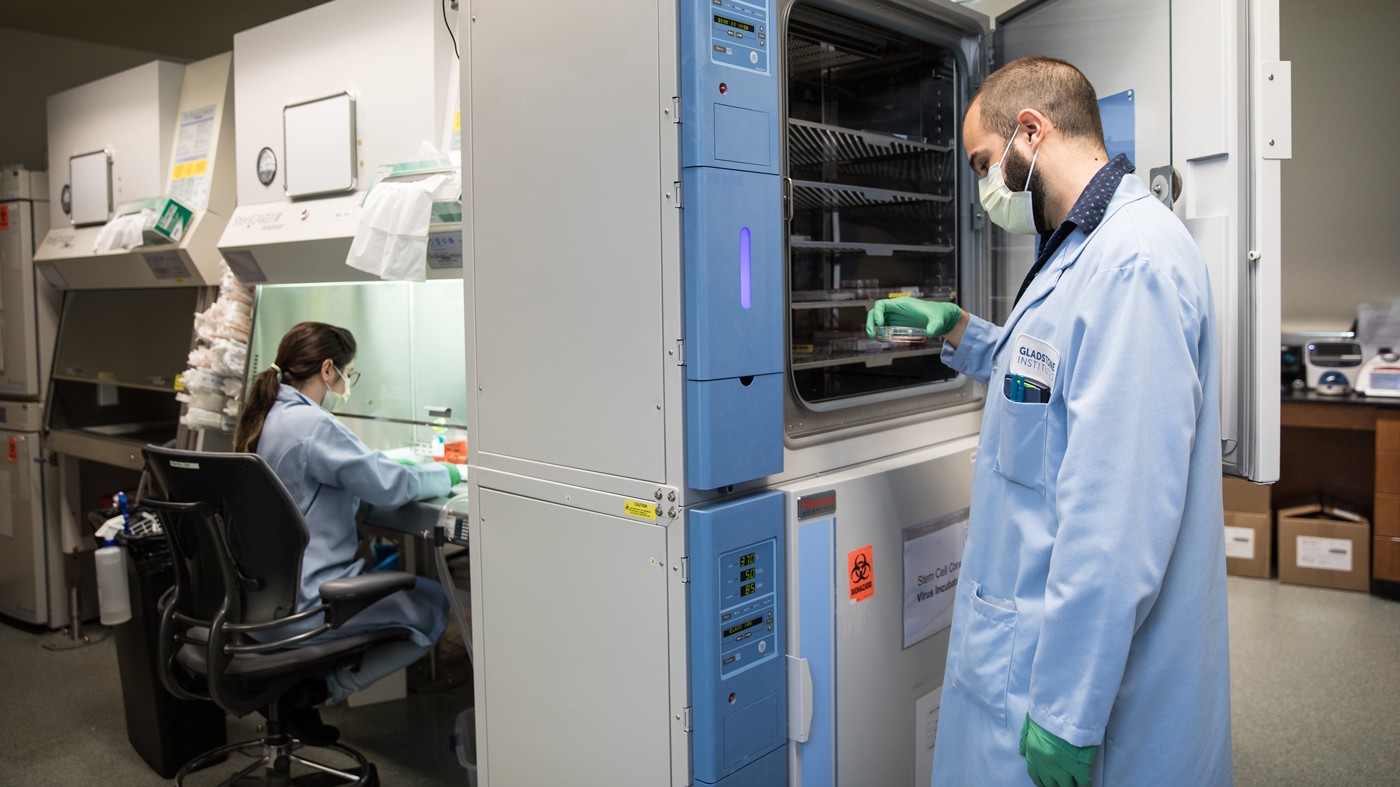
Fortunately, the tools we have here at Gladstone, specifically induced pluripotent stem cells (or iPS cells), enabled us to rise to this challenge.
How Exactly Did iPS Cells Help?
Perez-Bermejo: Human iPS cells are essentially stem cells that we can direct to become pretty much any type of cell in the body. We used iPS cells to grow human heart cells that were genetically identical in every way—except for their BAG3 genes. To do that, we used CRISPR genome editing technology to insert BAG3C151R or other BAG3 variants into some of the heart cells, allowing us to compare them head-to-head with cells that had a normal version of BAG3.
We already knew that the BAG3 protein plays a key role in helping heart cells deal with stress, so we applied a cardiotoxic drug to our lab-grown heart cells to see how they would respond.
What Did You Find?
Conklin: We found that cells with BAG3C151R were more resilient when facing the toxic drug than cells with the normal version of BAG3. And cells with two copies of BAG3C151R were even more resilient than cells with just one copy. This is strong evidence that BAG3C151R may directly contribute to a lower risk of heart failure in people.
“What Juan and the rest of our team achieved was kind of a molecular biology tour de force. This was a risky undertaking.”
Say the heart is like a car, and having a normal BAG3 gene is like getting the recommended oil change every several thousand miles; it’s going to help maintain your health. But having BAG3C151R may be like getting an oil change a little more often. For some people, that’s going to provide an extra benefit, and when you look at an entire population, getting the metaphorical oil changed just a little more often might have a big effect on the incidence of heart failure.
So How Do You Think the Protein Exerts This Protective Effect?
Perez-Bermejo: That’s the big question. But we’ve already found some clues. We know that the BAG3 protein performs its “quality control” function by interacting with many other proteins. So, we figured the protective effects of BAG3C151R might be reflected in changes to those interactions.
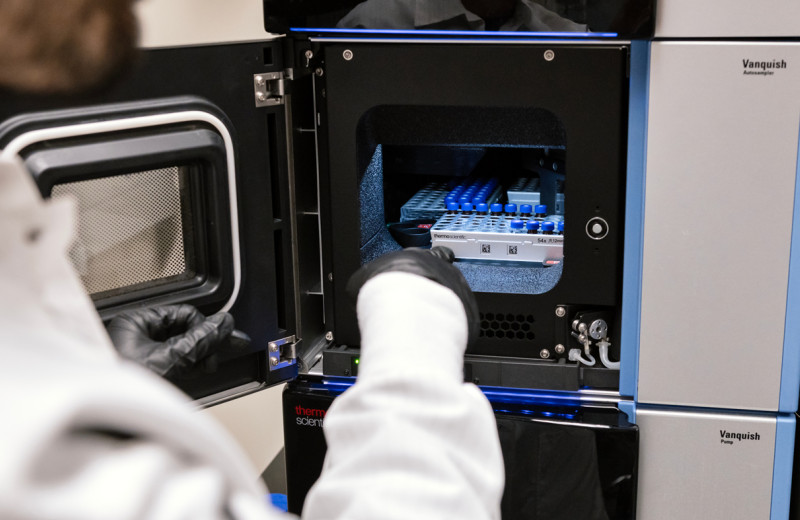
To explore this idea, we collaborated with Nevan Krogan, PhD, Gladstone senior investigator and co-author on the study, who has developed state-of-the art approaches for a technique called mass spectrometry. We used his methods to study BAG3 protein interactions in our iPS cell-derived heart cells.
We found that, compared to cells with the normal version of the BAG3 gene, cells with BAG3C151R showed an increase in certain interactions with other proteins, and a decrease in certain other interactions. Some of these proteins are already known to play a role in maintaining heart muscle strength, suggesting these particular interactions may be directly involved in the protective effects of BAG3C151R.
How Did It Feel to Confirm the Protective Effect of BAG3C151R in a Dish?
Perez-Bermejo: We were skeptical at first. The results were almost too good to be true. So, we did it again. And we did it again. Doing even a single iPS cell experiment can take months, so this project ultimately took a long time. But eventually, we repeated our experiments enough to be confident in the findings. And over the years, more and more genetic studies revealed this association in more and more people, which really encouraged us to keep going.
Conklin: What Juan and the rest of our team achieved was kind of a molecular biology tour de force. This was a risky undertaking. If it turned out that BAG3C151R didn’t have protective effects, we might have spent years on this project without a satisfying outcome.
How Could This Research Be Used to Address Heart Failure?
Perez-Bermejo: We expect this paper will be the foundation for many future studies working toward the development of treatments that mimic the protective effects of BAG3C151R in people with a predisposition for heart disease. You could imagine a small molecule drug that alters BAG3’s interactions with other proteins, or perhaps a gene therapy that actually introduces BAG3C151R into a person’s cells. But there is a long road ahead, and more research will be needed to clarify the molecular mechanism that drives this protection.
Conklin: Many companies—including Tenaya Therapeutics Inc., a company I co-founded with other Gladstone researchers—have already been working on BAG3-related treatments inspired by our knowledge of disease-causing BAG3 mutations. But this study marks the first time that a heart-protective association seen in population studies has been validated in the lab, paving the way for novel treatment strategies.
We believe this study will also serve as a roadmap for other researchers who want to take on the tremendous challenge of validating population-level protective associations in the lab.
The paper “Functional analysis of a common BAG3 allele associated with protection from heart failure” was published in the journal Nature Cardiovascular Research on June 26, 2023.
Other authors are Luke M. Judge, Christina L. Jensen, Kenneth Wu, Hannah L. Watry, Annie Truong, Matthew Carter, Wendy V. Runyon, Robyn M. Kaake, Ernst H. Pulido, Danielle L. Swaney, and Po-Lin So of Gladstone; and Jaclyn J. Ho and Mohammad A. Mandegar of Tenaya Therapeutics.
The work was supported by Fundación ‘La Caixa’ (100010434, LCF/BQ/US10/10230024), Bristol Myers Squibb (63376), the American Heart Association (15PRE2570008507, 13PRE1612001307), the National Institutes of Health (R01-HL130533, R01-HL13535801, P01-HL146366, F32AI127291), Tenaya Therapeutics, the Roddenberry Foundation, the California Institute of Regenerative Medicine (TG2-01160), and the National Institute of Child Health and Development (1K12HD072222).
Featured Experts
New Tool Reveals the Secrets of HIV-Infected Cells
New Tool Reveals the Secrets of HIV-Infected Cells
Developed by Gladstone scientists, HIV-seq could uncover new opportunities for treating HIV.
News Release Research (Publication) HIV/AIDS Infectious Disease Roan LabVitamin B3 Therapy Offers Hope for Fatal Childhood Disease
Vitamin B3 Therapy Offers Hope for Fatal Childhood Disease
A new framework that matches vitamins with genetic diseases helped uncover that high-dose vitamin B3 can dramatically extend survival in mice with NAXD deficiency.
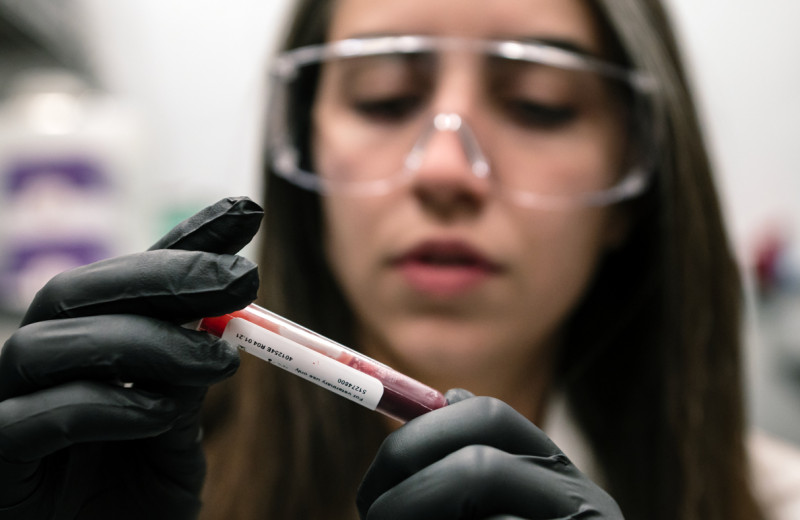
News Release Research (Publication) Rare Diseases Jain LabRed Blood Cells Soak Up Sugar at High Altitude, Protecting Against Diabetes
Red Blood Cells Soak Up Sugar at High Altitude, Protecting Against Diabetes
New study shows red blood cells act as hidden glucose sponges in low-oxygen conditions, explaining why people living at high altitude have lower diabetes rates and pointing toward new treatments.
News Release Research (Publication) Diabetes Jain Lab