Gladstone NOW: The Campaign Join Us on the Journey✕
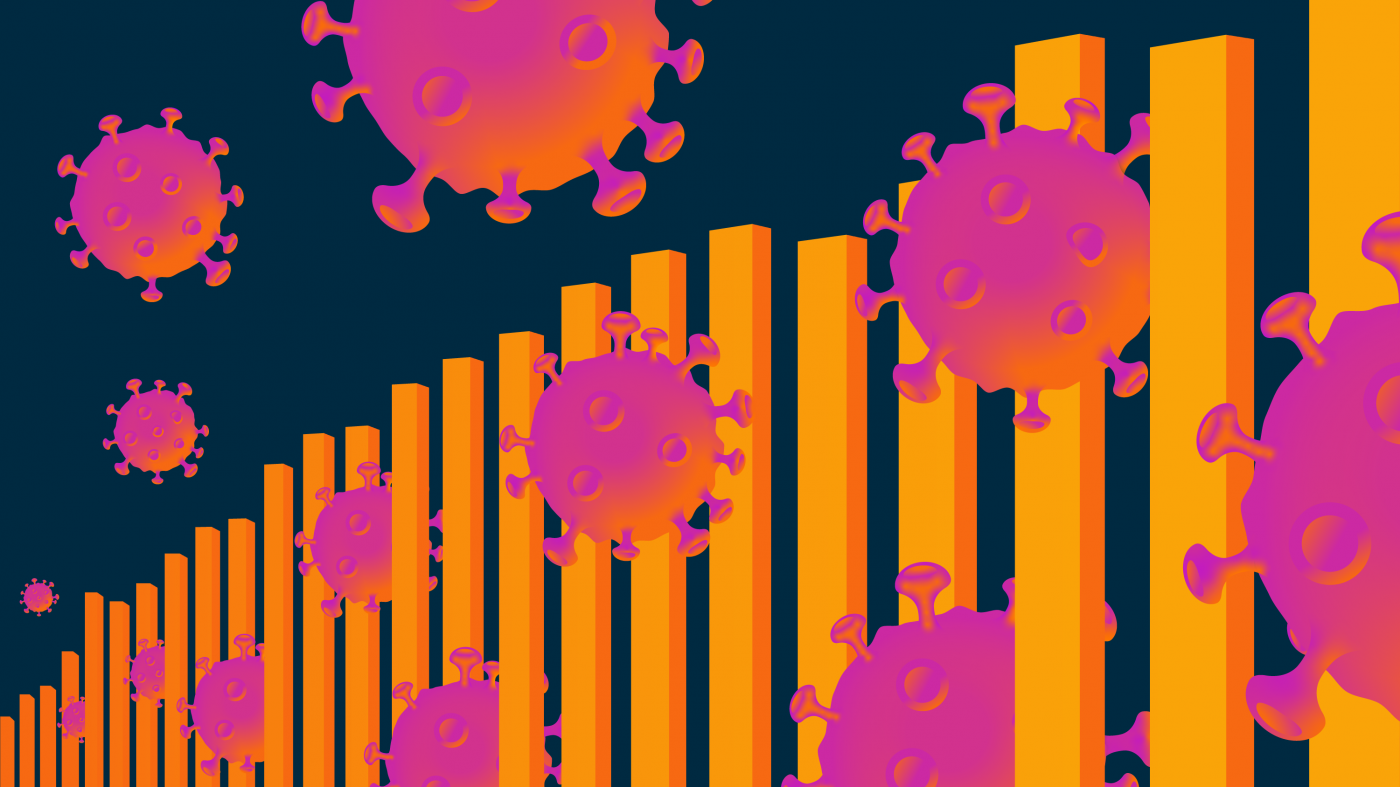
The highly infectious Delta variant and the slow vaccination rates in some parts of the US are resulting in an increased number of cases.
Update: This article was updated on August 2, 2021, to reflect the new mask guidance from the CDC for fully vaccinated individuals.
COVID-19 cases are surging again across much of the United States, fueled by the new Delta variant, lagging vaccination rates, and a relaxation of virus precautions.
The variant is a dangerous new version of the SARS-CoV-2 virus that appears able to infect with just 15 to 20 seconds of exposure. Emerging from the surge in India, Delta has rapidly out-competed earlier variants to become the dominant strain in the United States. Its formidable ability to infect people has already helped drive up new case counts in every US state, and led health officials in three California counties to reinstitute mask mandates.
So far, vaccines approved in the US protect against serious illness, hospitalization, and death from the new variant. But its emergence and rapid dominance show that it’s still too early to write the history of the COVID-19 pandemic. After spinning off at least four major variants in slightly more than 18 months, SARS-CoV-2 may yet have more tricks up its sleeve.
“We’re already in a new surge, and our numbers are steadily climbing,” says Melanie Ott, MD, PhD, director of the Gladstone Institute of Virology. “The difference between this surge and earlier ones is that it affects mostly unvaccinated people, and unfortunately, kids under 12 are among them. We need to vaccinate, vaccinate, vaccinate, and include kids as soon as possible.”
Virus Replication Errors Can Change Everything
In response to concern about the Delta variant, the Centers for Disease Control and Prevention (CDC) recently recommended that vaccinated and unvaccinated persons alike wear masks indoors in public if they are in areas with substantial or high viral transmission—which includes a majority of the US.
How can this be, just two months after fully vaccinated people were told they no longer needed to wear masks in most situations?
“It looks like the vaccines will still hold in terms of their primary function: preventing serious illness, hospitalization, and death.”
The answer involves the statistics of making copies. Viruses evolve for a single purpose: to make as many copies of themselves as possible in the cells of hosts—what virologists call replication. In making untold trillions and trillions of copies, however, occasionally the process produces errors in the sequence of genes in a new viral copy.
Most of those mistakes have no consequence, or even end up deactivating the mutated virus. But in a few instances, a mutation may create a viral strain with an evolutionary advantage over earlier variants. That may include an enhanced ability spread inside the body, or an ability to evade components of the immune system, such as protections created by vaccines or recovery from infection.
“It’s like being in Las Vegas—every once in a while, the virus hits the jackpot by finding a particular combination of mutations that makes it more infectious,” explains Warner Greene, MD, PhD, director of the Michael Hulton Center for HIV Cure Research at Gladstone. “If those improvements are significant, the mutated viruses become globally dominant, as happened with the Alpha variant originating in the United Kingdom, and now Delta, which was first identified in India during its recent devastating battle with COVID-19.”
There’s even an emerging “Delta Plus.” It’s a variant within a variant. It has all the mutations found in Delta, as well as an additional mutation that further helps the virus evade the protective effects of the immune system. Experts don’t yet know how it will behave, but hope it turns out not to be as infectious as the Delta variant.
The billion-dollar question worrying virologists is whether the viral mutation process will spin off a SARS-CoV-2 variant that can defeat the existing vaccines. So far, that hasn’t happened, and Greene believes the current vaccines are good enough to prevent it—if we can get them broadly distributed around the globe.
“With the vaccines we have now, we’re likely going to see more mild-to-moderate infections among fully-vaccinated individuals as the variants get better and better at infecting people,” he says. “But it looks like the vaccines will still hold in terms of their primary function: preventing serious illness, hospitalization, and death. This is the way most vaccines work, they don’t completely prevent infection, but they do prevent the emergence of disease.”
If Delta is bad news for the vaccinated, it’s terrible news for the unvaccinated.
In the United States, 97 percent of hospitalizations and 99.5 percent of deaths due to COVID-19 are occurring in unvaccinated individuals. And not only are case numbers surging with a more transmissible virus, but those who have avoided the vaccine jab can no longer count on protection from people who have gotten the shots. Vaccinated individuals may become infected and could unknowingly spread the virus to those who are unvaccinated, an issue that led the CDC to reinstitute its mask recommendations in late July.
“People developing mild illness or even asymptomatic infections could be carriers spreading the virus to others,” Greene says. “Most notably, the ones who are really going to be hit hard are the unvaccinated who are now vulnerable to a much more transmissible virus.”
Among the unvaccinated are children. While the vaccine has been approved in the US for adolescents ages 12 and over, younger children cannot yet receive it, making them particularly vulnerable to the new variant.
“We now have a virus that’s hitting harder at the younger age groups,” Greene says. “I’m eager for the vaccine trials underway now for children ages 5 and older to get results. Hopefully we can get these kids vaccinated soon.”
The Immune System’s One-Two Punch
Vaccination can stimulate the body to produce neutralizing antibodies that are able to rapidly knock out SARS-CoV-2 before it can establish an infection. But as the virus mutates, the effectiveness of those antibodies may decline. The same can occur with antibodies generated through a natural infection by SARS-CoV-2.
Fortunately, antibodies are only part of the protection story. The body’s immune system also uses T cells whose levels decline less quickly than antibodies. Although the T cells can’t keep the virus from launching an infection in the same way as the neutralizing antibodies, they are able to prevent the infection’s spread and may be critical for preventing severe disease.
So, while fully vaccinated people may get breakthrough infections with mild or no symptoms, they likely won’t see the inside of a hospital as a result.
“Unlike antibodies, T cells typically recognize actual infected cells, and in general, it’s more difficult for viruses to escape from the T cell–response,” says Nadia Roan, PhD, an associate investigator at Gladstone. “T cells recognizing SARS-CoV-2 also seem to be able to persist and self-renew, which is great news.”

New variants of SARS-CoV-2 can emerge as the virus acquires mutations to try to circumvent the immune response.
So, are antibodies or T cells more important to protecting people against the virus?
“Answering that is like trying to answer whether the string or woodwind section of an orchestra are more important,” she states. “They are equally important, and only with all the instruments being in sync is symphonic music created. Similarly, T cells and antibodies really have to work together for a functional immune system. A well-coordinated immune response—T cells working together with antibodies—is what’s needed to quickly eliminate the virus.”
Roan’s lab recently published a study on the impact of T cell activity on a patient’s outcomes from the virus. Her team found that in seriously ill persons who did not survive, the number of T cells that recognize the virus fell dramatically before death, while in those who survived, the counts rose until patients were discharged from the hospital.
The group continues to study the role of T cells and other immune cells, and the ultimate findings could provide an opening for drugs that may be effective during the later stages of COVID-19. That’s when a dysregulated immune response—rather than viral replication—seems to be the main problem, damaging the lungs and other organs even after the virus is long gone.
“The thought is that if natural immunity or therapeutics kick in early enough to prevent uncontrolled viral replication, that could prevent the virus from initiating the messed-up immune response,” Roan says. “But if you wait too long, some individuals will have this over-the-top inflammatory response that might actually be what kills them.”
Ironically, she notes, a growing immunity in the population can also drive the development of mutations that may help the virus evade vaccines.
“Besides the pressure to replicate faster, another kind of evolutionary pressure imposed on the virus is driven by the immune system,” she says. “When the virus was mutating at the very beginning of the pandemic, there wasn’t much immune-mediated pressure because not many people had been exposed to the virus and no one was vaccinated. Now, you have a lot of people who have some form of immunity to the virus, and that immunity can drive mutations.”
Specifically, when the virus infects a person who has some level of immunity, it adapts to this environment by acquiring mutations that can allow it to circumvent the immune response. When this virus infects the next person, it may show more immune resistance. Fortunately, none of the SARS-CoV-2 variants have evolved to completely overcome the immune responses elicited by the current vaccines.
What Happens in Other Countries Doesn’t Stay There
Controlling SARS-CoV-2 in the United States will require controlling it everywhere. With the pandemic raging around the world, there’s just too much opportunity for successful mutants to develop, become dominant, and spread.
“The virus is just getting started,” warns Ott. “If we don’t get case numbers under control nationally and internationally, the chances are very high that we will continue to see more nasty variants develop.”
Greene notes that the measure of transmissibility, known as “R-naught (R0),” has been steadily increasing. The original SARS-CoV-2 strain had an R0 value between 2.5 and 3, meaning each infected individual would transmit the virus, on average, to 2.5 to 3 other persons. The Delta variant has an R0 estimated to be between 6 and 8.
As the infectivity of the virus increases with variants like Delta, it becomes less likely that we can reach herd immunity, which happens when a large enough percentage of individuals with natural or vaccine-induced immunity could protect the unvaccinated from seeing the virus.
“The next few weeks will tell us how states like Mississippi, Louisiana, Tennessee, Missouri, Arkansas, Florida, Idaho, and Wyoming—which have low vaccination rates and an increasing number of infections—will be affected,” says Greene.
“Wearing a mask is still a very effective mitigation tool. I will continue to wear masks if I’m unsure about the vaccination and infection status of those around me.”
In addition, vaccines available in other countries vary, and some appear to be less effective against variants than the vaccines approved in the United States, Greene adds.
“Any time the virus has an opportunity to replicate at a high level, it’s going to spin out variants, and the most infectious variant will be the next one to take over,” he says. “So, if we’re not all protected, none of us are truly protected.”
If vaccinating to herd immunity in the US seems difficult, it’s much more of a challenge globally. The mRNA vaccines (from Pfizer/BioNTech and Moderna) must be transported and stored under arctic-like conditions that are not readily available in many countries, and providing two shots would tax many health care systems beyond their capabilities. That means vaccinating the world will require the use of many different vaccine platforms, including those needing less stringent storage conditions.
“Currently, less than 1.1 percent of people in low income countries have received even a first vaccine dose,” Greene says. “A vaccine like the one made by Johnson & Johnson that works as a single shot and doesn’t require super-cold storage may be the most effective for a global vaccination program.”
Hold Onto Those Masks
Ott, Greene, and Roan agree: Wearing masks is advisable, even for fully-vaccinated people when they are in crowded indoor places.
“Wearing a mask is still a very effective mitigation tool,” says Ott. “I will continue to wear masks if I’m unsure about the vaccination and infection status of those around me.”

Gladstone virologists encourage every eligible individual to get a COVID-19 vaccine as a way to help stop the creation of new variants and put an end to the current pandemic.
A major concern about even mild and moderate infection in unvaccinated individuals, and potentially in vaccinees, is whether it can result in the development of a condition known as “long COVID” or post-acute COVID-19 syndrome. It’s estimated that as many as a third of unvaccinated people infected with the virus suffer long-lasting symptoms, including difficulty breathing, irregular heartbeat, “brain fog,” loss of taste and sense of smell, and/or joint pain. These effects can linger for months after people recover from the acute infection.
“There’s currently no research on whether long COVID can appear in fully vaccinated individuals who suffer a breakthrough infection,” Greene says. “In general, the severity of infection doesn’t seem to play a major role in determining whether individuals will experience long-term symptoms.”
“A lot of these lingering symptoms negatively affect quality of life, sometimes in debilitating ways,” says Roan. “This is something we need to better understand. The root cause of long COVID is unknown, and is likely multifactorial. One possibility is that there may be some lingering virus around that creates constant low-grade inflammation.”
Women seem more likely to suffer from long COVID, which is the opposite of the more severe infection and acute death from COVID-19 seen in men. But there have been reports of some long COVID subjects improving after vaccination.
The US has all the advantages of plentiful vaccine protection against SARS-CoV-2 and a robust health care system to administer it. This makes Gladstone virologists all the more disappointed that vaccination campaigns have slowed dramatically.
“I’m glad to see high rates of vaccination in some areas, but disappointed to see there is still significant vaccine hesitancy,” says Greene. “Science has given us an incredibly safe and effective vaccine that can put this pandemic firmly in our rearview mirror. But right now, it’s in our blind spot.”
Support Our COVID-19 Research Efforts
Gladstone scientists are moving quickly to respond to the coronavirus outbreak. Help us end this pandemic.
Gladstone’s Scientific Highlights of 2025
Gladstone’s Scientific Highlights of 2025
From fundamental insights to translational advances, here’s how Gladstone researchers moved science forward in 2025.
Gladstone Experts Alzheimer’s Disease Autoimmune Diseases COVID-19 Neurological Disease Genomic Immunology Cardiovascular Disease Data Science and Biotechnology Infectious Disease Conklin LabScience in Seconds | Researchers Pinpoint Key Gene Behind Heart Defects in Down Syndrome
Science in Seconds | Researchers Pinpoint Key Gene Behind Heart Defects in Down Syndrome
In this video, Gladstone scientists share how they used stem cells, gene editing, and AI to identify a gene driving heart defects in Down syndrome—and how reducing its levels in mice restored normal heart development, offering hope for future treatments
Gladstone Experts Cardiovascular Disease Data Science and Biotechnology Pollard Lab Srivastava Lab AI Big Data CRISPR/Gene Editing Human Genetics Stem Cells/iPSCsScience in Seconds | The Thinking Microscope: Research Powered by an AI Brain
Science in Seconds | The Thinking Microscope: Research Powered by an AI Brain
In this video, Steve Finkbeiner and Jeremy Linsley showcase Gladstone’s groundbreaking “thinking microscope”—an AI-powered system that can design, conduct, and analyze experiments autonomously to uncover new insights into diseases like Alzheimer’s, Parkinson’s, and ALS.
Gladstone Experts ALS Alzheimer’s Disease Parkinson’s Disease Neurological Disease Finkbeiner Lab AI Big Data