Gladstone NOW: The Campaign Join Us on the Journey✕

Jae Kyu Ryu (right) and his colleagues discover new links between lymphoma growth and leaks in the blood-brain barrier.
In people with central nervous system (CNS) lymphoma, cancerous B cells—a type of white blood cell—accumulate to form tumors in the brain or spinal cord, often in close proximity to blood vessels. This disease is quite rare, but individuals who are affected have limited treatment options and often experience recurrence.
Previous research has linked the severity of CNS lymphoma to abnormal leaks in the blood-brain barrier, a protective system that allows some substances to pass from the bloodstream to the brain, while blocking others. However, the specific molecular details of this link have been murky.
Now, Gladstone researchers have shown in mice that CNS B-cell lymphoma cells cluster at sites where there is a leak in the blood-brain barrier. They also found that a blood protein called fibrinogen, which normally participates in blood clotting, promotes this clustering.
“Our findings link, for the first time, fibrinogen with CNS B-cell lymphoma, shedding new light on mechanisms of lymphoma growth in the brain that could be further explored as a treatment target,” says senior author Jae Kyu Ryu, PhD, staff research scientist at Gladstone Institutes.
The study was just published in The American Journal of Pathology.
Homing in on Fibrinogen’s Critical Role
CNS B-cell lymphoma is new territory for Ryu, but central to his research interest on the role of the blood-brain barrier in neurological diseases. His path to lymphoma research began when he and colleagues at Gladstone and UC San Francisco (UCSF) discovered that fibrinogen can leak through the blood-brain barrier in the brain of patients with B-cell lymphoma.
In parallel, James Rubenstein, MD, PhD, a professor at UCSF and co-author on the new study, had been studying the fluid that surrounds the brain and spinal cord to find clues on how B-cell lymphoma develops. He previously showed that, for patients with B-cell CNS lymphoma, this fluid harbors unusually high levels of proteins involved in blood clotting—including fibrinogen.
“With these clues in hand, I wanted to collaborate with Dr. Rubenstein and the UCSF Helen Diller Family Comprehensive Cancer Center and apply my expertise in blood-brain barrier leaks to determine more precisely how they might contribute to the development of CNS B-cell lymphoma,” says Ryu, who is also an assistant professor of neurology at UCSF and a member of the newly founded Gladstone-UCSF Center for Neurovascular Brain Immunology.
In the first step of the study, the researchers observed abundant buildup of fibrinogen around CNS lymphoma tumors in tissues from both human patients and a mouse model of the disease. Thanks to bioinformatics tools, the scientists identified fibrinogen and other blood-clotting proteins in the brain fluid of B-cell lymphoma patients connected with tumor-associated alterations in biochemical pathways. Next, they used cutting-edge microscopy techniques to track cells in the mouse brains.
“Using live imaging of the mouse brain, we found that the cells accumulated at sites of leakage in the blood-brain barrier and tended not to stray from the leaks,” says Justin Chan, first author of the study and undergraduate research intern at Gladstone, who is now a resident physician at the School of Medicine at the University of California, Irvine.
Tying it all together, the team finally showed that CNS lymphoma cells can stick to fibrinogen, but not to virtually every other protein found in mouse blood.
“That was kind of an ah-ha moment that pinpointed fibrinogen as a key protein that allows CNS B-cell lymphoma cells to adhere to the leakage sites in the brain,” Ryu says.
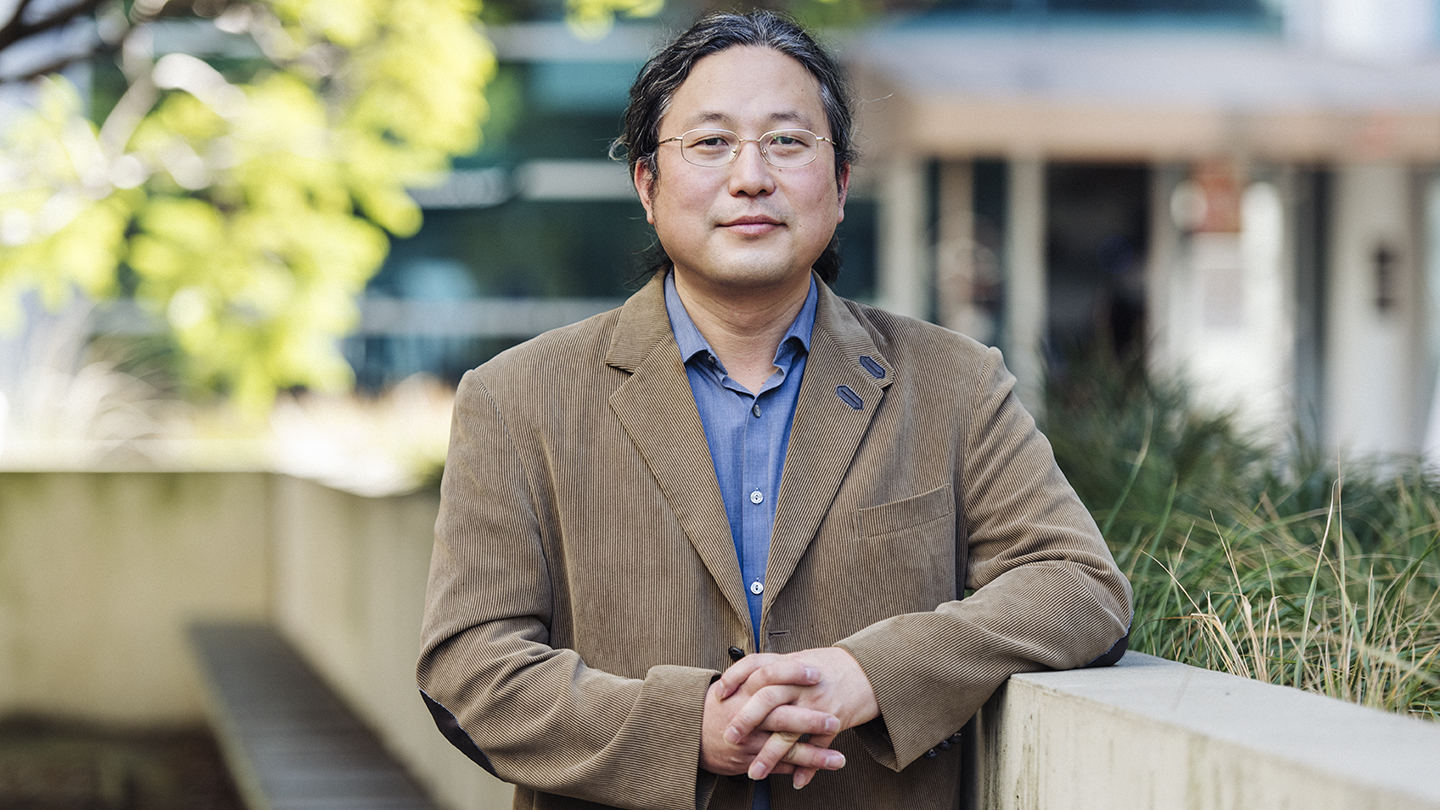
Ryu's latest study sheds light on lymphoma growth in the brain and could be used to explore a potentially new target for treatment.
“Fibrinogen is a common thread among multiple neurological and peripheral inflammatory diseases,” says study co-author Katerina Akassoglou, PhD, who is the director of the Gladstone-UCSF Center of Neurovascular Brain Immunology, a senior investigator at Gladstone, and a professor of neurology at UCSF. “The new findings may reveal unanticipated mechanisms at the intersection of the vascular, brain, and immune interface in brain B-cell lymphoma, as well as novel targets for therapies and biomarkers.”
An Attractive New Target for Lymphoma Treatment
The study’s results suggest that fibrinogen could potentially be targeted to treat CNS B-cell lymphoma. Existing drugs that disrupt fibrinogen’s activity may at first seem an appealing option. However, these drugs could excessively disturb the protein’s beneficial blood-clotting role and lead to dangerous side effects, such as increased risk of tumor metastasis.
However, Ryu and colleagues are uniquely qualified to tackle this challenge: they have already developed an immunotherapy that blocks the specific role played by fibrinogen in neurological diseases, without disrupting the blood-clotting process.
The next step will be to better understand the molecular pathway by which fibrinogen promotes B-cell lymphoma in the brain, and to determine whether that role can be separated from the blood-clotting process.
“Our new findings provide an exciting foundation for future studies on developing strategies to precisely block the lymphoma-promoting activity of fibrinogen,” adds Ryu. “This could help us identify very specific aspects of fibrinogen’s activity that could be targeted safely and effectively.”
For Media
Julie Langelier
Associate Director, Communications
415.734.5000
Email
About the Study
The study, “Blood Coagulation Factor Fibrinogen in Tumor Pathogenesis of Central Nervous System B-Cell Lymphoma,” was published on February 16, 2021 in the journal The American Journal of Pathology.
Other authors on the study include Gladstone researchers Mario Merlini and Andrew Mendiola, and UCSF researcher Hua-Xin Gao.
The researchers were supported by the National Institute of Neurological Disorders and Stroke (grant R35NS097976), the National Cancer Institute (grant R01CA139‐83‐01A1), the Leukemia and Lymphoma Society, the National Multiple Sclerosis Society, Race to Erase MS, the American Heart Association, the Conrad N. Hilton Foundation, and the Simon Family Trust.
About Gladstone Institutes
Gladstone Institutes is an independent, nonprofit life science research organization that uses visionary science and technology to overcome disease. Established in 1979, it is located in the epicenter of biomedical and technological innovation, in the Mission Bay neighborhood of San Francisco. Gladstone has created a research model that disrupts how science is done, funds big ideas, and attracts the brightest minds.
Featured Experts
Gladstone Scientist Nadia Roan Elected to American Academy of Microbiology
Gladstone Scientist Nadia Roan Elected to American Academy of Microbiology
Roan has made great strides in understanding how persistent viruses including HIV cause disease and how immunity to viruses shapes human health.
Awards News Release COVID-19 HIV/AIDS Infectious Disease Roan LabRed Blood Cells Soak Up Sugar at High Altitude, Protecting Against Diabetes
Red Blood Cells Soak Up Sugar at High Altitude, Protecting Against Diabetes
New study shows red blood cells act as hidden glucose sponges in low-oxygen conditions, explaining why people living at high altitude have lower diabetes rates and pointing toward new treatments.
News Release Research (Publication) Diabetes Jain LabDisrupted Boundary Between Cell Types Linked to Common Heart Defects
Disrupted Boundary Between Cell Types Linked to Common Heart Defects
Gladstone scientists identified a cellular boundary that guides heart development and revealed how disrupting it can lead to holes in the heart’s wall.
News Release Research (Publication) Congenital Heart Disease Cardiovascular Disease Bruneau Lab