Gladstone NOW: The Campaign Join Us on the Journey✕
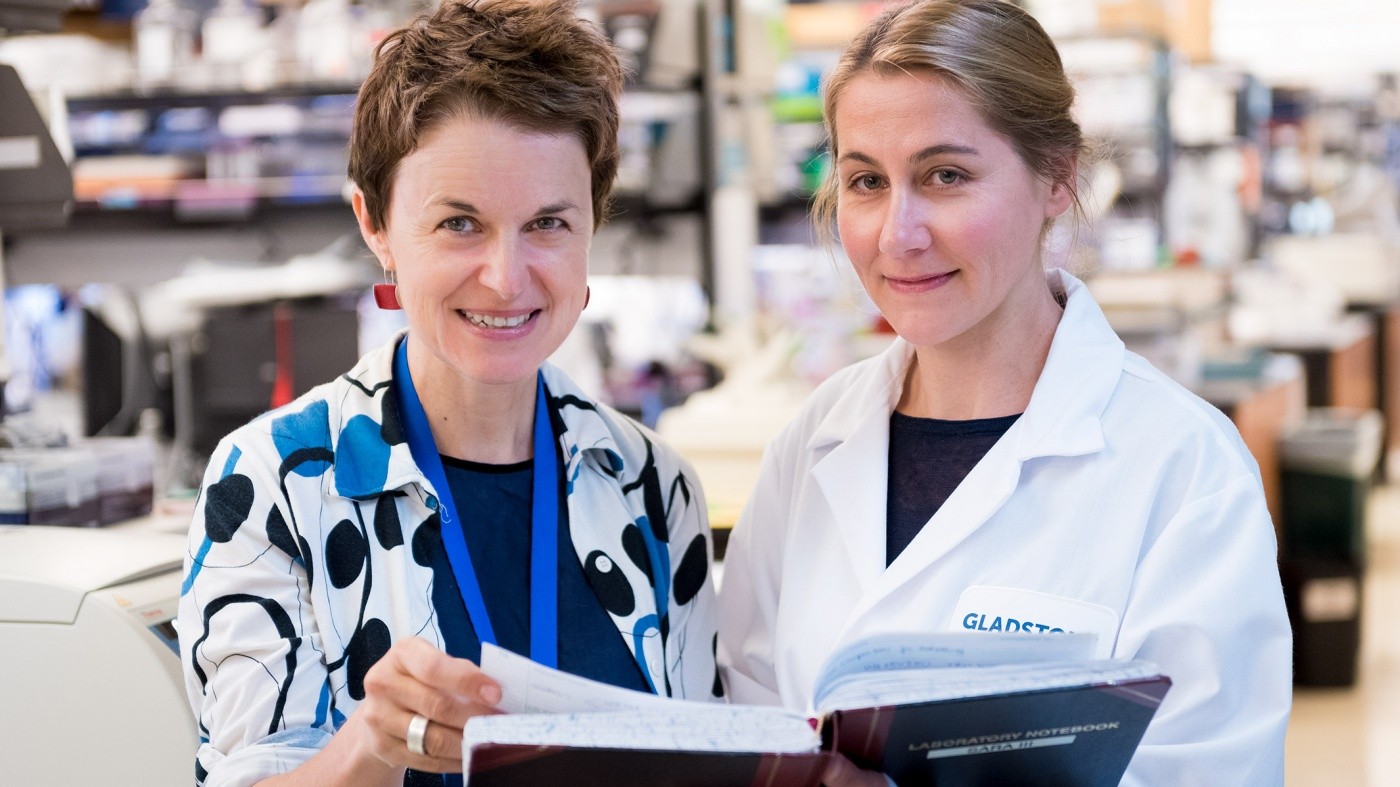
Melanie Ott (left) and Daniela Boehm (right) uncovered a new therapeutic target for flushing out latent HIV. [Photo: Chris Goodfellow, Gladstone Institutes]
Scientists at the Gladstone Institutes discovered that an enzyme called SMYD2 could be a new therapeutic target for flushing out the HIV that hides in infected individuals. Overcoming this latent virus remains the most significant obstacle to a cure.
While drug therapy allows people living with HIV to lead a relatively normal life, it also comes with adverse effects. In addition, patients must stay on the drugs for life to prevent the virus hiding in their body from reactivating. In the early stages of infection, HIV hides in viral reservoirs in a type of immune cells called T cells. This dormant, or latent, virus can then spontaneously reactivate and rekindle infection if drug therapy is stopped.
To eliminate HIV latency, scientists are exploring a “shock and kill” strategy that would use a combination of drugs to wake up the dormant virus, then act with the body’s own immune system to eliminate the virus and kill infected cells. Previous research has had limited success in efficiently reactivating latent HIV, so scientists are working to find new, more effective drugs.
“Our study focused on a class of enzymes called methyltransferases, which have emerged as key regulators of HIV latency,” explained Melanie Ott, MD, PhD, a senior investigator at Gladstone and lead author of the study published in the scientific journal Cell Host & Microbe. “These enzymes have also become increasingly important in disease development, particularly cancer, and efforts have intensified to develop specific pharmacological inhibitors targeting them.”
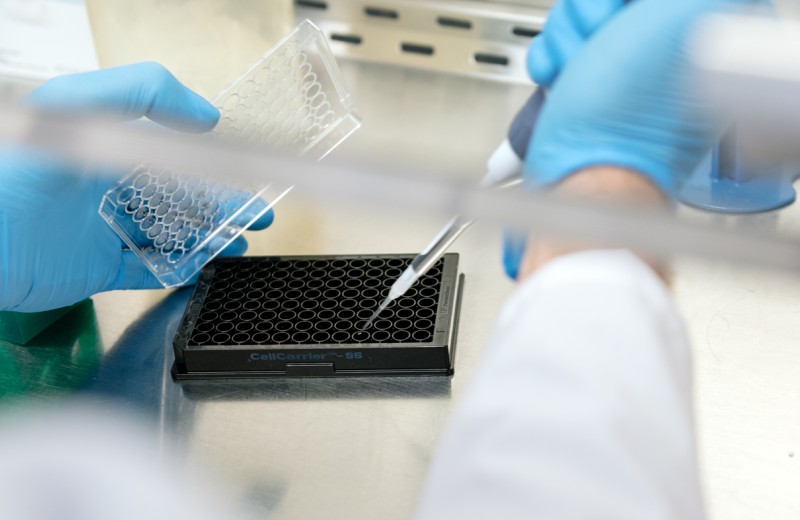
“We systematically screened over 50 methyltransferases to determine which ones regulate latency in infected T cells,” said Daniela Boehm, postdoctoral scholar in the Ott laboratory and first author of the study. “We identified SMYD2 as a regulating enzyme, and found that inhibiting it reactivates, or wakes up, latent cells. SMYD2 could therefore be used as a therapeutic target in the shock and kill strategy.”
Although SMYD2 was not previously considered a target for HIV, pharmacological inhibitors are already being developed against this enzyme due to its effect on various cancer tumors.
“Our findings offer new biological and mechanistic insights into how latency functions,” added Ott, who is also a professor in the Department of Medicine at the University of California, San Francisco (UCSF). “They also suggest potential translational applications. Through a valuable collaboration with our industry partners, we obtained samples of small molecules in pre-clinical development that target SMYD2 and could potentially activate latent HIV.”
In collaboration with Warner C. Greene, MD, PhD, the researchers tested the small molecules that inhibit SMYD2 in human cells.
“We found that these small SMYD2 inhibitors were able to activate the virus in latently infected T cells isolated from HIV patients,” said Greene, senior investigator and director of the Gladstone Institute of Virology and Immunology.
“Our findings provide the basis for a new model of HIV latency wherein SMYD2 contributes to durably repressing the latent virus,” said Ott. “They also underscore the emerging ties between cancer and HIV treatment through shared pharmacological targets. Though we are still far from a human application, it is exciting to know that data from this study might readily connect with clinical efforts.”
Other Gladstone scientists on the study include Mark Jeng, Gregory Camus, Andrea Gramatica, Roland Schwarzer, Jeffrey R. Johnson, Philip A. Hull, Mauricio Montano, Naoki Sakane, Sara Pagans, and Nevan J. Krogan. Collaborators from the University of California, San Francisco, and AstraZeneca also took part in the study.
This research project was funded by the UCSF–Gladstone Center for AIDS Research (P30 AI027763), the amfAR Institute for HIV Cure Research (109301), the California HIV/AIDS Research Program (F13-373GI-316), the James B. Pendleton Charitable Trust, as well as grant support from the Collaboratory of AIDS Researchers for Eradication (U19 AI096113), and the National Institutes of Health (RO1AI083139, RO1 DA043142, and P50 GM082250).
40 Years of HIV Research: Celebrating the Career of Virologist Warner Greene
40 Years of HIV Research: Celebrating the Career of Virologist Warner Greene
Colleagues look back on Warner Greene's 40 year career
Gladstone Experts History HIV/AIDS Infectious Disease Greene LabTips from Virologists to Face the “Tripledemic” This Holiday Season
Tips from Virologists to Face the “Tripledemic” This Holiday Season
Gladstone scientists answer questions about the convergence of COVID-19, RSV, and the flu this winter
Gladstone Experts COVID-19 Infectious Disease Greene Lab Ott Lab Roan LabWhen Will This Pandemic End?
When Will This Pandemic End?
And other questions you have about Omicron and the pandemic
Gladstone Experts COVID-19 Infectious Disease Greene Lab Ott Lab Roan Lab