Gladstone NOW: The Campaign Join Us on the Journey✕

Gladstone scientists—including Ivana Vasic, seen here— show that barriers between stem cells play a crucial role in human development and offer a new potential route for fertility treatment.
As a human embryo grows, a set of molecules directs cells as they multiply and take on specific identities and spatial positions within the embryo. In one crucial step known as gastrulation, these signaling molecules guide a single layer of embryonic stem cells to form three layers of distinct cell types that will later become different parts of the body.
Now, researchers in the iPS Cell Research Center at Gladstone Institutes have shown that tight junctions between cells may play a critical role in gastrulation in human embryos.
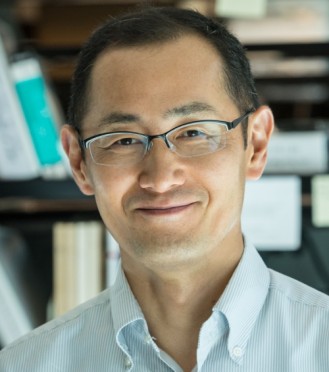
“This study has exciting implications for the way we design gastrulation models and other lab techniques for differentiating stem cells into specialized cell types,” says Shinya Yamanaka, MD, PhD, senior investigator at Gladstone and a senior author of the study published in the journal Developmental Cell. “The better we understand signaling mechanisms in embryos, the more easily we can recapitulate these processes in robust, reproducible ways.”
The team is already applying their results to develop novel techniques for transforming stem cells in a dish into human egg cells—a strategy that could one day be used for in vitro fertilization.
Discovery on the Edge
Gastrulation sets a foundation for the development of the entire human body. Researchers have found ways to recreate a simplified version of this fundamental process in a dish by starting with a layer of induced pluripotent stem cells, or iPS cells—adult cells that have been reprogrammed to mimic embryonic stem cells, meaning they can differentiate to become any cell type in the body.
Then, scientists add a protein called BMP4, a key signaling molecule in gastrulation, which causes the cells in the dish to begin to form the three layers of cells found in the embryo. However, since all of the cells appear to receive the same BMP4 signal, it has been unclear why some transform into one cell type while others become different cell types.
“This has been kind of a head scratcher in the field,” says Ivana Vasic, PhD, lead author of the study and a former postdoctoral researcher at Gladstone. “All these cells are either interpreting the same cue from BMP4 differently, or they’re not really getting the same cue.”
While creating a gastrulation model in the lab, Vasic observed that the iPS cells clustered together in the dish contain proteins that are the building blocks for tight junctions, which are barriers between cells. But she also noticed that the tight junctions don’t always actually assemble.
Yamanaka, Vasic, and their team found that growing the cells in a less-confined space allowed the tight junctions to assemble consistently. When they added BMP4 to the unconfined cells, they got their “aha” moment: only cells at the edge of the cluster received enough BMP4 to activate molecular pathways that would nudge them to become different layer cell types.
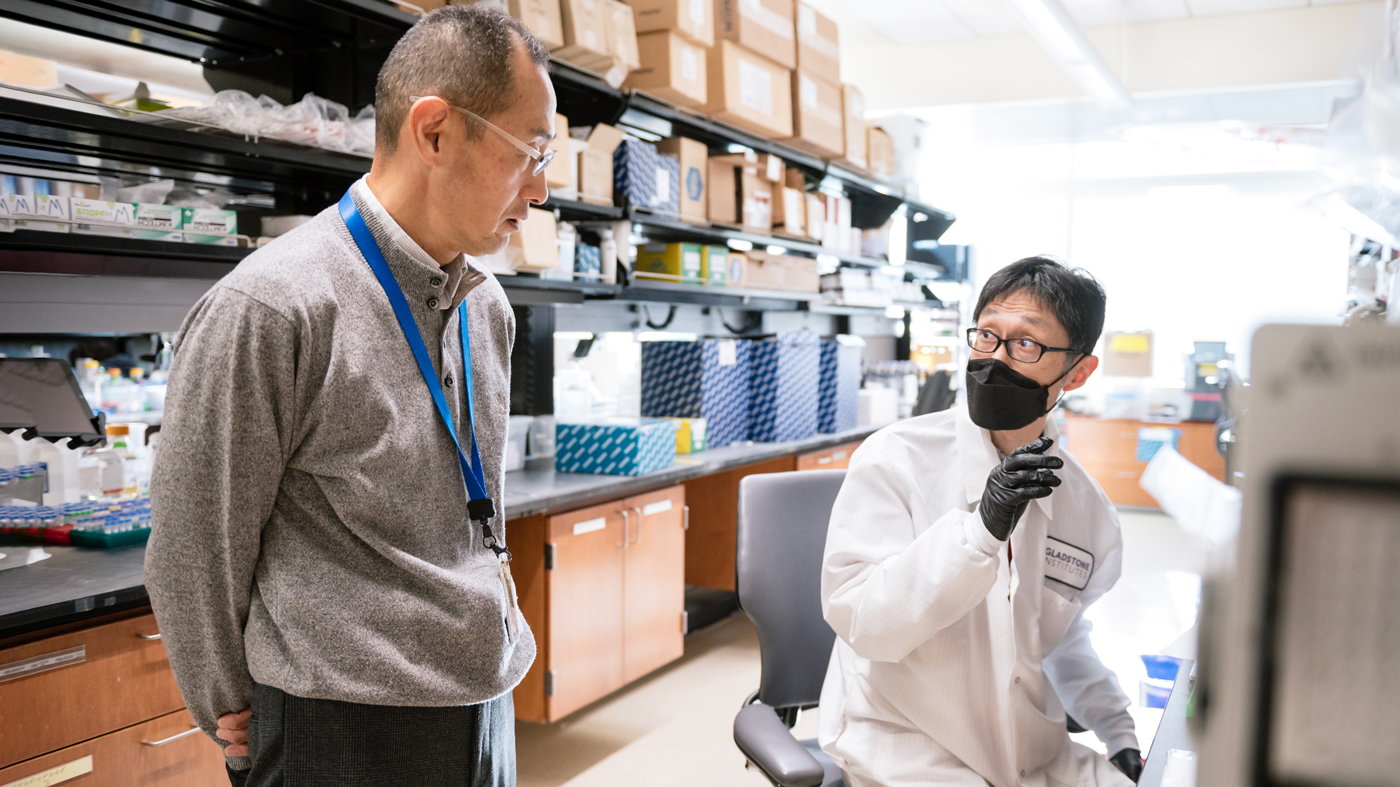
Yamanaka (left), Kiichiro Tomoda (right), and their colleagues found that the structure of stem cells is very important to how they receive differentiation signals.
“Tight junctions between adjacent cells seem to make them impervious to signals from BMP4,” Vasic says. “But the edge cells don’t have a buddy to form tight junctions with on their outer side, which means they are getting the strongest cues from BMP4.”
To confirm the importance of tight junctions in gastrulation, the researchers used CRISPR genome editing technology to suppress production of TJP1, a protein that is crucial for forming tight junctions in iPS cells. When they applied BMP4 to cells lacking the TJP1 protein, every single cell was activated, not just the edge cells.
“We showed that removing the tight junctions made all the cells respond to BMP4,” says Yamanaka, who is also a professor of anatomy at UC San Francisco, as well as director emeritus and professor at the Center for iPS Cell Research and Application (CiRA), Kyoto University, in Japan. “This suggests that tight junctions block cells from responding to signals in gastrulation models, and more fundamentally, that the structure of cells is very important to how they receive differentiation signals.”
“Broadly speaking, this study demonstrates how perturbations to innate properties of iPS cells can modulate their sensitivity to extracellular cues and alter their cell fate trajectory,” says Todd McDevitt, PhD, former senior investigator at Gladstone and a senior author of the study. “This principle could be a game changer for unlocking the potential of iPS cells to produce more homogeneous populations of differentiated cells for therapeutic applications.”
Creating Egg Cells in a Dish
The team then took a closer look at the identity of the cells that had been activated by BMP4 after perturbing tight junction formation.
“We stumbled upon a very exciting finding: it turns out that we could create a special type of cell called a primordial germ cell-like cell,” Vasic says. “These are stem cells produced in a lab that resemble the human precursors of sperm and egg cells.”
“We’re essentially trying to recapitulate the biological process of egg production, so that we can generate eggs that people could use for in vitro fertilization.”
Researchers have long sought a reliable method for generating primordial germ cell-like cells, but struggled to produce them from iPS cells. Vasic and her colleagues had discovered that suppressing TJP1 could form the basis of a novel method to efficiently produce these unique cells.
Now, Vasic has founded a new company, Vitra Labs, to apply this method in a possible new strategy for treating women’s infertility.
“We’re essentially trying to recapitulate the biological process of egg production, so that we can generate eggs that people could use for in vitro fertilization,” Vasic says. “It’s kind of the cherry on top of our study.”
For Media
Julie Langelier
Associate Director, Communications
415.734.5000
Email
About the Study
The paper “Loss of TJP1 disrupts gastrulation patterning and increases differentiation toward the germ cell lineage in human pluripotent stem cells” was published in the journal Developmental Cell on June 23, 2023.
Other authors are Ashley R.G. Libby, Emily A. Bulger, David Zalazar, Martina Z. Krakora Compagno, and Kiichiro Tomoda of Gladstone; and Annie Maslan and Aaron Streets of UC San Francisco.
The work was supported by the Core Center for iPS Cell Research, Research Center Network for Realization of Regenerative Medicine, Japan Agency for Medical Research and Development (JP21bm0104001); the iPS Cell Research Fund; Kyoto University’s on-site laboratory initiative; Hiroshi Mikitani; Marc and Lynne Benioff; the L.K. Whittier Foundation; the Roddenberry Foundation; the National Heart, Lung, and Blood Institute; the National Institutes of Health (U01-HL100406, U01-HL098179, R01-HL130533, and R01-HL135358); the California Institute for Regenerative Medicine (LAI-C1408015); and Emergent Behaviors of Integrated Cellular Systems consortium (CBET0939511).
About Gladstone Institutes
Gladstone Institutes is an independent, nonprofit life science research organization that uses visionary science and technology to overcome disease. Established in 1979, it is located in the epicenter of biomedical and technological innovation, in the Mission Bay neighborhood of San Francisco. Gladstone has created a research model that disrupts how science is done, funds big ideas, and attracts the brightest minds.
Featured Experts
Disrupted Boundary Between Cell Types Linked to Common Heart Defects
Disrupted Boundary Between Cell Types Linked to Common Heart Defects
Gladstone scientists identified a cellular boundary that guides heart development and revealed how disrupting it can lead to holes in the heart’s wall.
News Release Research (Publication) Congenital Heart Disease Cardiovascular Disease Bruneau LabGene Editing Strategy Could Treat Hundreds of Inherited Diseases More Effectively
Gene Editing Strategy Could Treat Hundreds of Inherited Diseases More Effectively
Scientists at Gladstone show the new method could treat the majority of patients with Charcot-Marie-Tooth disease.
News Release Research (Publication) Neurological Disease Conklin Lab CRISPR/Gene EditingGenomic Maps Untangle the Complex Roots of Disease
Genomic Maps Untangle the Complex Roots of Disease
Findings of the new study in Nature could streamline scientific discovery and accelerate drug development.
News Release Research (Publication) Marson Lab Genomics Genomic Immunology