Gladstone NOW: The Campaign Join Us on the Journey✕

Cell models of infection are invaluable tools in investigating how viruses spread.
For most people living in the US today, the COVID-19 pandemic seems unprecedented; the scale at which it is affecting modern life is certainly unmatched in recent history. But for researchers who spent decades studying viruses and how they can wreak havoc on the human population, the SARS-CoV-2 virus carries a sense of familiarity. In addition to parallels with recent epidemics—SARS, MERS, and Ebola, to name a few—they see shadows of the early HIV crisis in today’s trying times.
“The situation is certainly reminiscent of what happened in the 1980s when HIV emerged,” says Gladstone Senior Investigator Melanie Ott, MD, PhD. “No one knew exactly how the virus worked and we had very little to offer patients who were in end-stage disease.”
Ott and others whose careers have revolved around studying HIV are now finding that their experiences and the tools they developed during that epidemic have valuable implications for COVID-19.
“The difference of course is that HIV never blocked our economy or kept everyone in the country at home,” says Ott. “But a lot of the lessons that have been learned from HIV are very applicable here.”
A Shared Sense of Urgency
In 1981, when the first HIV patient was seen at the National Institutes of Health (NIH), Gladstone Senior Investigator Warner Greene, MD, PhD, was a trainee. No one knew at that point what caused this targeted attack on the immune system; it would be 3 years before HIV was identified as the viral cause of AIDS, and much longer before combination antiviral therapy became available. When he moved to San Francisco to direct the new Gladstone Institute of Virology and Immunology in 1991, Greene served as an attending physician on the wards of San Francisco General Hospital, and recalls that all of his patients were HIV positive and all were dying.

Senior Investigator Warner Greene is applying research techniques his team developed to study HIV to investigate the novel coronavirus.
Over time, this urgency helped drive a new push to study viruses, the development of new types of antiviral drugs, and spawned a new generation of immunology researchers inspired to solve diseases of the immune system. The years of research that followed shed new light on how the human body responds to viruses, what viral proteins are best to target therapeutically, and what makes a vaccine successful or not. This research is, in part, what made it possible for scientists to so quickly isolate and characterize SARS-CoV-2.
“Our understanding of viruses in general have certainly been expanded by our studies of HIV,” says Greene. “It is probably the best studied pathogen in the world, and our history with HIV is going to help guide scientists to attack this coronavirus in effective ways.”
Greene’s own work has focused on how the human body responds to HIV. The symptoms of AIDS and destruction of immune cells, he has shown, have more to do with an overzealous response by the immune system than the virus itself.
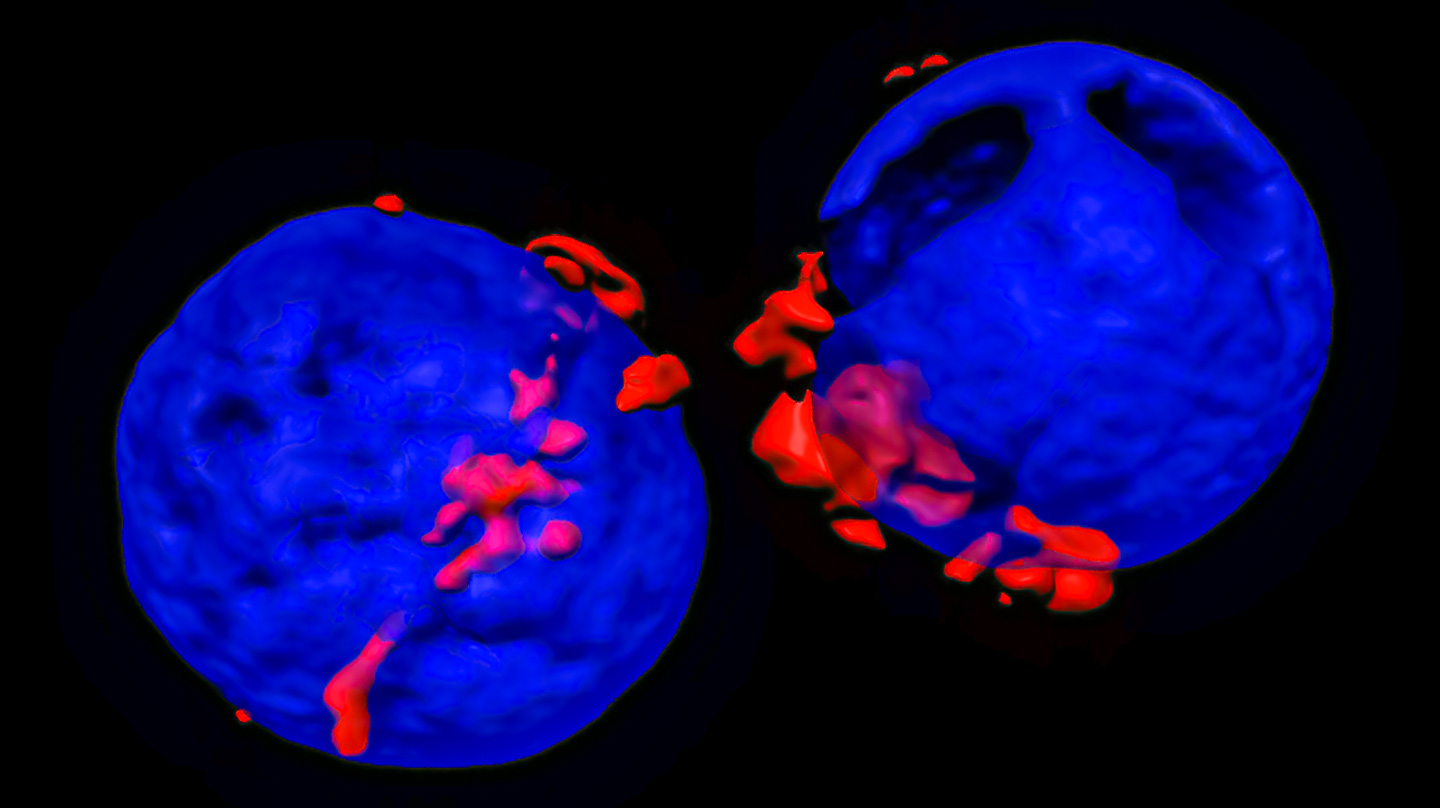
Cell models of infection are invaluable tools in investigating how viruses spread.
“Viruses are professional pirates,” says Greene. “They get inside cells and commandeer all the intracellular machinery. They cannot live for long free of cells.”
Several years ago, Greene’s research team at Gladstone created a new and easy way to monitor how HIV gets inside human cells in the first place. When specially engineered HIV particles infect cells, the cells light up with fluorescence. The researchers discovered that they could use this approach to study not only the entry process of HIV, but any other viruses they wanted as well, by substituting a set of proteins from the virus in question.
Now, Greene’s team is adapting this technology to study SARS-CoV-2. Not only can this approach help them better understand the coronavirus, but Greene says it can be used to screen drugs. If a drug is effective at stopping SARS-CoV-2 from infecting human cells, the cells will no longer light up with fluorescence when mixed with the viral particles. He also plans to use the technology to study blood from people who have recovered from COVID-19; he can determine whose blood contains antibodies that specifically recognize the entry process of SARS-CoV-2, which may protect them from re-infection.
In addition, he and his collaborators are looking at blocking peptides that might be effective therapeutics. Gladstone Senior Investigator Katerina Akassoglou, PhD, and Greene are also exploring effects of SARS-CoV-2 on the neurovasculature, hoping to better understand the increased incidence of stroke seen in COVID-19. Finally, Greene and his colleagues are looking for new approaches to block the cytokine storm that can have lethal consequences late in the course of disease. A similar host response occurs during HIV infection and contributes to the progressive loss of CD4 T cells.
New Challenges with COVID
Ott was a neurologist practicing in Frankfurt, Germany, during the AIDS crisis, and her experience treating patients infected with the virus motivated her to go back to school and study virology. For the last 30 years, she’s studied not only HIV but hepatitis C, Zika, dengue, and other viruses. But over the past few months, she’s shifted her focus to COVID-19.
“We were working with the right tools that we felt could be very useful for SARS-CoV-2,” says Ott.
Over the past few years, Ott’s group, along with Gladstone Senior Investigator Jennifer Doudna, PhD, has been developing a rapid, mobile phone–based HIV self-test that detects the virus’s RNA. Now, they’ve begun applying the same approach to a test for SARS-CoV-2.

Senior Investigator Melanie Ott’s experience caring for patients during the AIDS crisis inspired her to devote her career to studying viruses.
Ott’s lab has also worked with organoids—miniature versions of human organs that can be grown in the lab using stem cells. For instance, she uses intestinal organoids to study how HIV causes gut inflammation, as well as to screen potential drugs for their efficacy. If a drug can reverse the signs of disease in an intestinal organoid, that’s a good sign that it can treat disease in a functioning human intestine. Since COVID-19 primarily infects the lungs, Ott is studying COVID-19 using lung organoids.
In many ways, COVID-19 is harder to study than HIV, Ott says. “Coronaviruses are much bigger than HIV,” she explains. “They are the largest of the RNA viruses and have lots and lots of gene products.”
In addition, research involving active COVID-19 requires more precautions than HIV, since SARS-CoV-2 can be passed through the air. That’s why Ott’s team will use a biosafety level-3 (BSL-3) lab for any experiments using live virus.
“Because some pathways are shared between many viruses, our hope is that we develop a drug—or a repertoire of drugs—that are not only effective against COVID-19, but future virus epidemics as well,” says Ott.
Support Our COVID-19 Research Efforts
Gladstone scientists are moving quickly to respond to the coronavirus outbreak. Help us end this pandemic.
Gladstone’s Scientific Highlights of 2025
Gladstone’s Scientific Highlights of 2025
From fundamental insights to translational advances, here’s how Gladstone researchers moved science forward in 2025.
Gladstone Experts Alzheimer’s Disease Autoimmune Diseases COVID-19 Neurological Disease Genomic Immunology Cardiovascular Disease Data Science and Biotechnology Infectious Disease Conklin LabScience in Seconds | Researchers Pinpoint Key Gene Behind Heart Defects in Down Syndrome
Science in Seconds | Researchers Pinpoint Key Gene Behind Heart Defects in Down Syndrome
In this video, Gladstone scientists share how they used stem cells, gene editing, and AI to identify a gene driving heart defects in Down syndrome—and how reducing its levels in mice restored normal heart development, offering hope for future treatments
Gladstone Experts Cardiovascular Disease Data Science and Biotechnology Pollard Lab Srivastava Lab AI Big Data CRISPR/Gene Editing Human Genetics Stem Cells/iPSCsScience in Seconds | The Thinking Microscope: Research Powered by an AI Brain
Science in Seconds | The Thinking Microscope: Research Powered by an AI Brain
In this video, Steve Finkbeiner and Jeremy Linsley showcase Gladstone’s groundbreaking “thinking microscope”—an AI-powered system that can design, conduct, and analyze experiments autonomously to uncover new insights into diseases like Alzheimer’s, Parkinson’s, and ALS.
Gladstone Experts ALS Alzheimer’s Disease Parkinson’s Disease Neurological Disease Finkbeiner Lab AI Big Data



