Gladstone NOW: The Campaign Join Us on the Journey✕

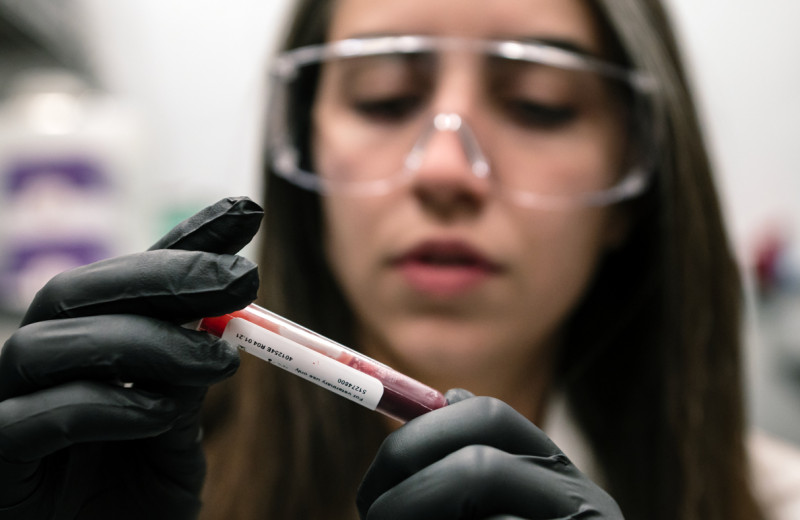
Gladstone scientist Dr. Sheng Ding has exposed more chameleon-like qualities of the human skin cell, using chemical cocktails to turn skin cells into fully functional brain, heart, liver, and insulin-producing pancreas cells. His revolutionary technique gives fresh hope for effective therapies to patients across the spectrum. [Photo: Chris Goodfellow]
Diseases of the brain and heart. Liver failure. Diabetes. Conditions for which, at present, there are no cures. In his laboratory at the Gladstone Institutes, young chemist Sheng Ding, PhD, the William K. Bowes, Jr. Distinguished Investigator at Gladstone, is working tirelessly to change this through his pioneering new approach.
“For so many illnesses, the underlying cause often boils down to the fact that cells needed to keep an organ healthy have died, or were never there to begin with,” says Deepak Srivastava, MD, director of the Roddenberry Stem Cell Center at Gladstone. “Dr. Ding has found an entirely new way to replenish the very cells lost to disease.”
More Efficient, Effective Approach to Stem Cell Creation
Dr. Ding’s approach is one of a kind, but his work builds on a revolutionary discovery by another Gladstone scientist—Nobel Laureate Shinya Yamanaka, MD, PhD, who in 2007 revealed a process for transforming adult skin cells into cells that look and act like embryonic stem cells.
Dr. Yamanaka did so by inserting four genes, now known as the “Yamanaka factors,” into adult skin cells. These genes effectively rewired the adult cell, taking it back to a stem cell-like, or pluripotent state, meaning it had the potential to generate almost all human cell types. The so-called induced pluripotent stem cells, or iPS cells, could then be directed to develop into virtually any cell type in the body.
Dr. Ding’s method, by contrast, has a few key twists. Instead of using a set of genes to induce the cellular transformation, he relies primarily on pharmaceutical compounds, known as “small molecules.” These small molecules interact with the cell’s molecular properties and guide it backwards in time—not to pluripotency, but to an intermediate, precursor state.
Dr. Ding’s approach mitigates some risks that come with iPS cell creation. For example, newly generated iPS cells could fail to fully mature into the desired cell type, resulting in an incomplete transformation, and incompletely transformed cells, when injected into a patient, could possibly lead to tumors if not removed. By never entering pluripotency, the cells resulting from Dr. Ding’s process more closely resemble the body’s native cells and are therefore less likely to induce tumor growth.
“Instead of taking skin cells back to their stem cell-like beginnings, we used small molecules to take them only part way,” explains Dr. Ding. “By relying more on small molecules, we also reduced our need to insert multiple genes. In the end, this helped us to generate a large reservoir of cells that could more efficiently be coaxed into becoming the cells we were looking to generate.”
The advantages of this approach began to emerge in 2011, when Dr. Ding announced that he had used his “chemical reprogramming” method to convert human skin cells into brain cells. The benefits of his method were then made abundantly clear in recent months, when Dr. Ding and his colleagues, in a scientific trifecta, published three separate studies illustrating the power of his approach to treat three more increasingly prevalent, and potentially lethal, conditions.
Type 1 Diabetes
Type 1 diabetes is defined by the destruction of pancreatic beta-cells, which produce the hormone insulin. While the disease can be managed with daily monitoring and insulin injections, patients must endure a relentless management schedule that is by no means fail-safe: many still experience loss of sight, kidney failure, and more. A permanent solution—beta-cell replacement—has long been the goal of stem cell scientists. And in the February 6 issue of Cell Stem Cell, Dr. Ding and his colleagues, using the method he pioneered, demonstrated their capacity to do just that.
In lab experiments on animal models, performed in collaboration with Matthias Hebrok, PhD, director of the Diabetes Center at UCSF, Dr. Ding and his team used a carefully screened set of small molecules to transform skin cells into early-stage pancreas cells. They then transplanted these early-stage cells into mice modified to have hyperglycemia (high glucose levels), a key indicator of diabetes.
Eight weeks later, the team noted its most surprising discovery: these early-stage cells had, on their own, given rise to functional, insulin-secreting beta-cells. “As early as one week post-transplant, the animals’ glucose levels started to decrease, gradually approaching near-normal levels,” notes Gladstone Postdoctoral Scholar and Ding lab member Ke Li, PhD, the study’s lead author. “And when we removed the transplanted cells, we saw an immediate glucose spike, uncovering a direct link between the transplanted cells and glucose levels.”
Not only did the team’s results point to the power of chemical reprogramming to generate a complete transformation, they also revealed that this type of regenerative therapy could use the patient’s own cells to regenerate the cells lost to disease.
Heart Disease
Worldwide, 23 million heart-attack survivors—with six million in the United States alone—are living with heart failure, a chronic condition in which the heart, having lost muscle during the attack, does not beat at full capacity. In the February 20 issue of Cell Reports, Dr. Ding and his team again demonstrated their successful use of chemical reprogramming, this time to regenerate beating heart cells.
In an earlier discovery, Dr. Srivastava’s team at Gladstone showed that inserting three-to-seven genes into a skin cell can transform it into a beating heart cell, without passing through the pluripotent state. This approach successfully created new heart muscle from scar-forming cells in hearts of animals, pointing to a new method for regeneration that harnesses cells already present in the damaged organ.
“Because gene therapy may carry certain risks, we set out to see if we could perform a similar transformation with small molecules, thereby eliminating—or at least reducing—our reliance on genetic manipulation,” says Dr. Ding.
The research team, which included Gladstone Postdoctoral Scholar Haixia Wang, PhD, the study’s lead author, identified a four-molecule chemical cocktail that could guide the skin cells into becoming more like heart cells. And when they added just a single gene to the mix, the clusters of heart-like cells matured even further and began to beat in sync, mimicking the behavior of native beating heart cells. Together, the teams of Drs. Srivastava and Ding are confident that they will soon find a way to eliminate the need for genes entirely, thus using only a cocktail of small molecules to generate beating heart muscle and regenerating damaged hearts.
Liver Disease
In the final study, Dr. Ding and his colleagues turned to the liver, the study of which has been particularly troubling for stem cell biologists. In collaboration with researchers at the University of California, San Francisco (UCSF), Dr. Ding and his team—once again harnessing the power of chemical reprogramming—surmounted previous challenges to generate fully mature, functional liver cells.
In prior studies, scientists had difficulty with maintaining the survival of stem cell-derived liver cells once transplanted into existing liver tissue. But the Gladstone-UCSF team determined a process for solving this problem. Writing in the February 23 issue of Nature, the team revealed they had once again used small molecules to effect a near-complete cellular transformation.
As with their two earlier studies, Dr. Ding and his UCSF collaborators, led by Holger Willenbring, MD, PhD, associate director of the UCSF Liver Center, utilized small molecules, along with very few genes, to transform adult skin cells into early-stage liver cells. After observing the transformation in a petri dish, they injected these cells into the livers of animal models to see if the transformation could become complete.
“Two months post-transplantation, we noticed a boost in human liver protein levels, an indication the transplanted cells were becoming mature,” says Saiyong Zhu, PhD, a Postdoctoral Scholar at Gladstone and the California Institute for Regenerative Medicine who was among the study’s lead authors. “Nine months later, the cells had shown no signs of slowing down and were functioning like normal liver cells.”
The researchers had found the right combination of factors required to successfully regenerate liver tissue—offering a potential treatment for those at risk of liver failure.
The Road Ahead
“What Dr. Ding has shown with these three studies is nothing short of extraordinary,” says Dr. Srivastava. “He’s revealed that, with the precise set of small molecules, one cell type can be transformed into another, almost at will. As his methods continue to improve, I have no doubt we will see a heavier reliance on small molecules. And from there, the possibilities are endless.”
At just 40 years old, Dr. Ding sees a long, bright future ahead as he continues to improve and refine his method. He hopes that one day a simple pill, containing the right chemical cocktail, will help a patient regrow the cells lost to disease.
“When people think about the power of regenerative medicine, they often think of scientists growing organs in the lab to transplant into patients,” says Dr. Ding. “But what we are trying to do is to give the human body the necessary tools to regenerate lost tissue—all on its own.”
Red Blood Cells Soak Up Sugar at High Altitude, Protecting Against Diabetes
Red Blood Cells Soak Up Sugar at High Altitude, Protecting Against Diabetes
New study shows red blood cells act as hidden glucose sponges in low-oxygen conditions, explaining why people living at high altitude have lower diabetes rates and pointing toward new treatments.
News Release Research (Publication) Diabetes Jain LabRoddenberry Gift Ushers Gladstone Stem Cell Research into the Future
Roddenberry Gift Ushers Gladstone Stem Cell Research into the Future
The path to medical breakthroughs lies in bold, ambitious science
Donor Stories Institutional News Spinal Cord Injuries Alzheimer’s Disease Diabetes Roddenberry Stem Cell Center Bruneau Lab Ding Lab Huang Lab McDevitt LabScientists Discover Drug that Increases “Good” Fat Mass and Function
Scientists Discover Drug that Increases “Good” Fat Mass and Function
Anti-cancer drug prevented less weight gain and caused mice to burn more calories thanks to higher levels of metabolism-boosting brown fat.
Ding Lab Metabolism Diabetes