Gladstone NOW: The Campaign Join Us on the Journey✕
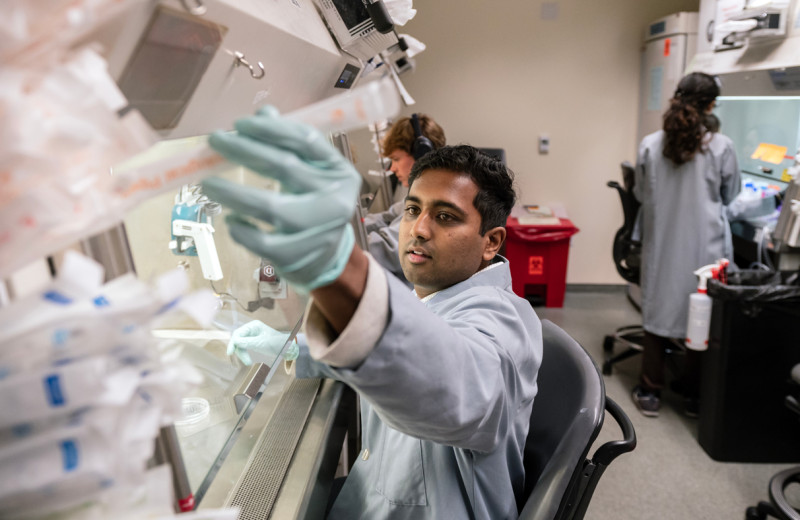
Gladstone scientists are using innovative methods to improve stem cell engineering and scale-up tissue manufacturing. [Image: Gladstone Institutes]
The world of biomedical research experienced a revolution when Nobel Prize-winner and Gladstone senior investigator Shinya Yamanaka, MD, PhD, discovered a way to produce induced pluripotent stem cells (iPSCs). Made from a person’s skin or blood cells, these stem cells can be reprogrammed into virtually any type of cell in the body, including heart, liver, brain, kidney, and pancreas cells. iPSCs are used to create disease models that facilitate research and drug discovery, and they may lead to the discovery of new treatments for deadly conditions like heart disease, diabetes, and neurodegenerative disease.
But manufacturing stem cells is challenging. The process is tedious, time-consuming and expensive, and out of a million skin cells that start out in the lab, in some cases, only one percent may fully develop into the appropriate cells. What’s more, there are no universally accepted protocols in place, resulting in problems with variability and reproducibility.
While the first clinical trials with iPSCs have only just begun, scientists are optimistic the cells will be widely used in the clinic within the next five years. When stem cell therapies become a reality, up to a billion cells may be needed to treat each patient. However, at this time, scientists do not have ways to produce enough cells consistently, posing a fundamental problem of supply and demand.
As in other manufacturing industries, reliable, efficient stem cell production will be necessary to meet the market demand. Funding agencies, including the US government, recognize the glaring need for better technologies to engineer biological products, and the Department of Defense recently issued a call for proposals on cell and tissue manufacturing. Forward-looking researchers at the Gladstone Institutes are answering this call, working to solve the stem cell supply problem by pursuing innovative ways to improve stem cell engineering.
Making the Right Kind of Cells
Sheng Ding, PhD, a senior investigator at Gladstone, is working to circumvent this problem by creating organ-specific stem cells that can reproduce themselves, offering an unlimited supply of healthy new cells. Ding’s lab discovered how to intercept stem cells that are turning into heart cells at a middle stage during their conversion when they have already been designated as cardiac stem cells but can still self-replicate. When transplanted into a heart, these induced expandable cardiovascular progenitor cells (ieCPCs) organically develop into mature heart cells.
“Cardiac progenitor cells could be ideal for heart regeneration,” said Ding. “They are the closest precursor to functional heart cells, and, in a single step, they can rapidly and efficiently become heart cells, both in a dish and in a live heart. With our new technology, we can quickly create billions of these cells in a dish and then transplant them into damaged hearts to treat heart failure.”
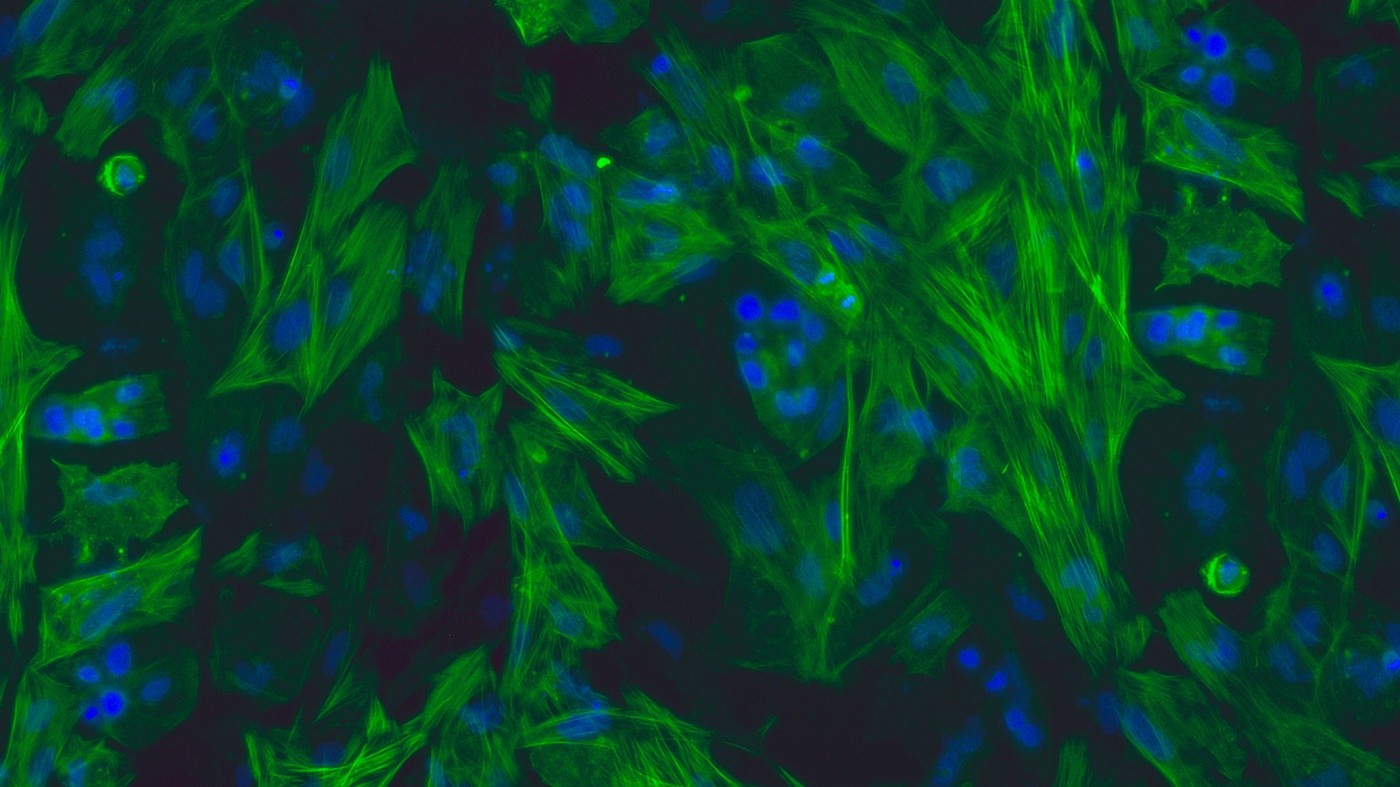
Ding’s team used drugs to catch and maintain heart stem cells at the cardiac precursor state before they developed into fully functional heart cells. These ieCPCs expanded exponentially over a dozen generations, creating billions of cells, enough to potentially treat dozens of patients. The new cells are particularly appealing as a way to treat heart failure because they can develop into any of the three different types of heart cells—cardiomyocytes, endothelial cells, and smooth muscle cells—all of which are needed to replenish a damaged heart. In support of this hypothesis, when the scientists injected the cells into mice that had suffered a heart attack, the ieCPCs spontaneously developed into mature heart cells, dramatically improving heart function.
Scaling Down Requirements
Researchers face another manufacturing concern—how to reliably grow individual cells into three-dimensional tissues that more closely resemble the tissues in organs. These bits of tissue are better for drug testing and have important potential clinical applications. However, engineering large numbers of three-dimensional organ tissues requires billions of cells, again presenting a supply problem for iPSC manufacturing.
As an alternative to scaling up the production of iPSCs, scientists in the lab of Gladstone senior investigator Bruce Conklin, MD, have reduced the size of the tissue samples, making them cheaper and more efficient to manufacture. The researchers developed a new method that uses a unique dog bone-shaped mold to help iPSC generated heart cells to aggregate, stretch into elongated muscle fibers, and self-organize into three-dimensional tissues. The new engineering technique requires a thousand-fold fewer cells than earlier methods, making it an easier, cheaper, and more efficient system. The resulting “micro” heart muscle can be used to model disease and test drugs. Because these cells have been engineered to exactly match specific disease mutations, it also opens the door for a precision medicine approach to treating heart disease.
“The beauty of this technique is that it is very easy and robust, but it still allows us to create three-dimensional miniature tissue samples that function like normal tissues,” explained Conklin. “Our research shows that these complex tissues can be created with a simple template that exploits these cells’ inherent tendency to self-organize. We think that the micro heart muscle will provide a superior resource for conducting research and developing therapies for heart disease.”
Leveraging Stem Cells Qualities
Gladstone senior investigator Todd McDevitt, PhD, is taking a different approach, exploring the possibility of reducing the need for stem cells. McDevitt’s lab is working to isolate and harvest the factors that stem cells secrete and turn them into drugs that leverage the cells’ self-replicating and pluripotent capabilities.
“We know that stem cells are unique in their ability to grow and divide and turn into other cells. Maybe it’s the factors they produce that give them these special capabilities,” said McDevitt. “If we can eliminate the need to transplant cells and simply deliver what they would secrete instead, we may be able to speed up the process of wound healing or even regenerate tissues without having to manufacture billions of cells for transplantation. As promising as stem cell transplant technology is, we also want options that reduce potential safety risks.”
The researchers have now used stem cell factors to successfully grow healthy new bone tissue, extracting the proteins the cells secrete in order to harness their regenerative power. To do so, they first transformed the stem cells into early bone cells. Next, they mined the essential factors produced by the cells that are necessary to regenerate new tissue. Finally, the researchers delivered these stem cell-derived factors into mouse muscle tissue, which facilitated new bone growth. This technology could provide a sustainable source for fresh tissue and reduce the risk of tumor formation that can arise with stem cell transplants.
Keeping Pace
Stem cell technology holds tremendously promising clinical potential, but equal to that promise is the challenge of production. If this technology is to advance from the laboratory to the patient, then manufacturing innovation must keep pace with the science. Gladstone scientists are dedicated to finding the answers to both. They will continue to seek novel solutions, ultimately revealing better treatments for a broad spectrum of human disease.
Gene Editing Strategy Could Treat Hundreds of Inherited Diseases More Effectively
Gene Editing Strategy Could Treat Hundreds of Inherited Diseases More Effectively
Scientists at Gladstone show the new method could treat the majority of patients with Charcot-Marie-Tooth disease.
News Release Research (Publication) Neurological Disease Conklin Lab CRISPR/Gene EditingGladstone’s Scientific Highlights of 2025
Gladstone’s Scientific Highlights of 2025
From fundamental insights to translational advances, here’s how Gladstone researchers moved science forward in 2025.
Gladstone Experts Alzheimer’s Disease Autoimmune Diseases COVID-19 Neurological Disease Genomic Immunology Cardiovascular Disease Data Science and Biotechnology Infectious Disease Conklin LabThe Genome Editing Playbook Is Different in Neurons
The Genome Editing Playbook Is Different in Neurons
The striking findings of a new study could influence how gene therapies are designed for many genetic diseases.
News Release Research (Publication) Neurological Disease Conklin Lab Doudna Lab CRISPR/Gene Editing