Gladstone NOW: The Campaign Join Us on the Journey✕

Swetansu Hota and his colleagues in the Bruneau Lab discovered, to their surprise, that removing one gene from developing heart cells suddenly makes them turn into brain cell precursors.
Imagine you’re baking a cake, but you run out of salt. Even with the missing ingredient, the batter still looks like cake batter, so you stick it in the oven and cross your fingers, expecting to end up with something pretty close to a normal cake. Instead, you come back an hour later to find a fully cooked steak.
It sounds like a practical joke, but this kind of shocking transformation is what really happened to a dish of mouse stem cells when scientists at Gladstone Institutes removed just one gene—stem cells destined to become heart cells suddenly resembled the precursors to brain cells. The scientists’ chance observation is upending what they thought they knew about how stem cells turn into adult cells and maintain their identity as they mature.
“This really challenges fundamental concepts about how cells stay the course once they embark on their path to becoming heart or brain cells,” says Benoit Bruneau, PhD, director of the Gladstone Institute of Cardiovascular Disease and a senior author of the new study published in Nature.
No Turning Back
Embryonic stem cells are pluripotent—they have the ability to differentiate, or transform, into every type of cell in a fully formed adult body. But it takes many steps for stem cells to give rise to adult cell types. On their path to becoming heart cells, for instance, embryonic stem cells first differentiate into mesoderm, one of three primitive tissues found in the earliest embryos. Further down the path, the mesoderm cells branch off to make bones, muscles, blood vessels, and beating heart cells.
It’s generally well accepted that once a cell has begun differentiating down one of these paths, it can’t turn around to choose a different fate.
“Pretty much every scientist who talks about cell fate uses a picture of the Waddington landscape, which looks a lot like a ski resort with different ski slopes descending into steep, separated valleys,” says Bruneau, who is also the William H. Younger Chair in Cardiovascular Research at Gladstone and a professor of pediatrics at UC San Francisco (UCSF). “If a cell is in a deep valley, there’s no way for it to jump across to a completely different valley.”
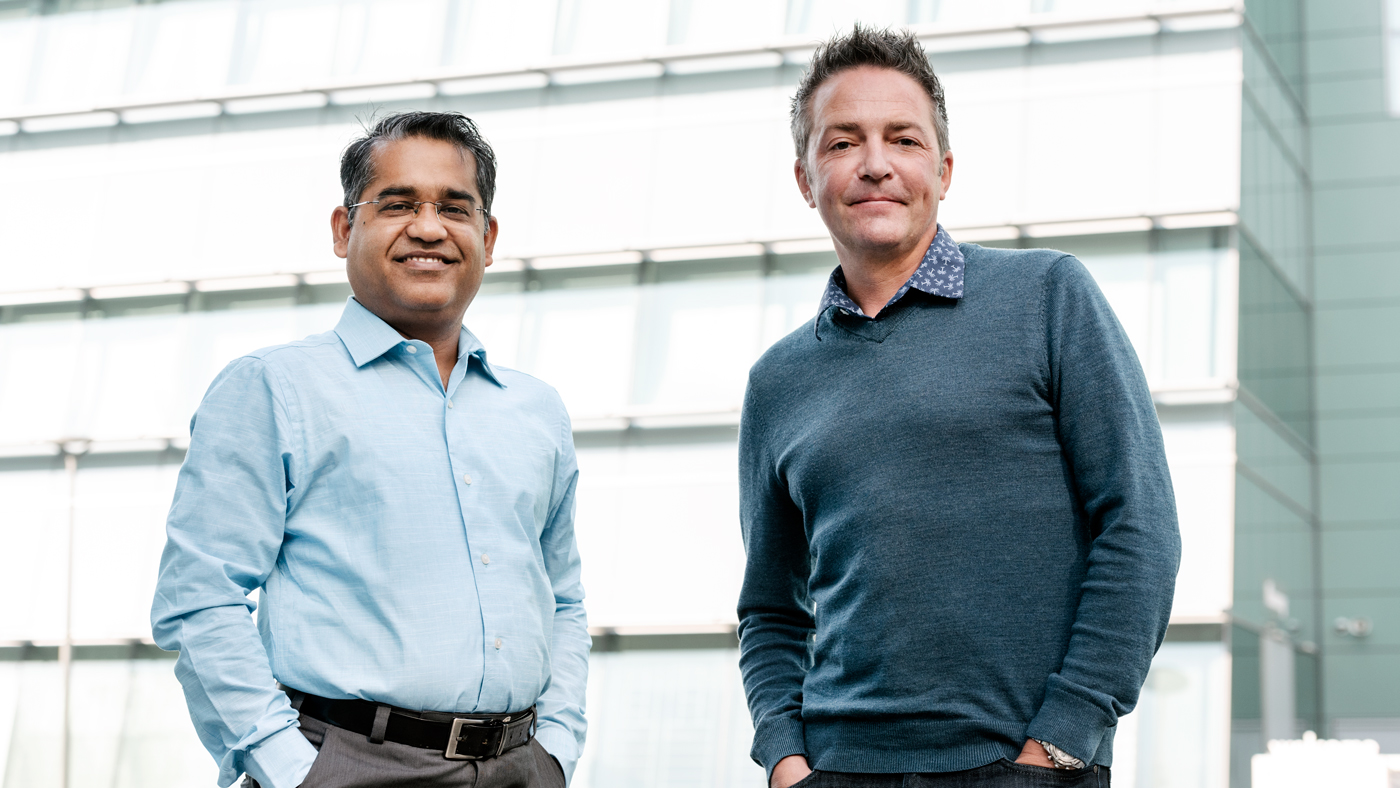
Swetansu Hota (left) and Benoit Bruneau (right) discovered that removing a protein called Brahma not only turned off genes required for heart cells, but also activated genes needed in brain cells.
A decade ago, Gladstone Senior Investigator Shinya Yamanaka, MD, PhD, discovered how to reprogram fully differentiated adult cells into induced pluripotent stem cells. While this didn’t give cells the ability to jump between valleys, it did act like a ski lift back to the top of the differentiation landscape.
Since then, other researchers have discovered that with the right chemical cues, some cells can be converted into closely related types through a process called “direct reprogramming”—like a shortcut through the woods between neighboring ski trails. But in none of these cases could cells spontaneously jump between drastically different differentiation paths. In particular, mesoderm cells could not become the precursors of such distant types as brain cells or gut cells.
Yet, in the new study, Bruneau and his colleagues show that, to their surprise, heart cell precursors can indeed transform directly into brain cell precursors—if a protein called Brahma is missing.
A Surprising Observation
The researchers were studying the role of the protein Brahma in the differentiation of heart cells, because they discovered in 2019 that it works together with other molecules associated with heart formation.
In a dish of mouse embryonic stem cells, they used CRISPR genome-editing approaches to turn off the gene Brm (the one that produces the protein Brahma). And they noticed that the cells were no longer differentiating into the normal heart cell precursors.
“After 10 days of differentiation, normal cells are beating rhythmically; they’re clearly heart cells,” says Swetansu Hota, PhD, first author of the study and a staff scientist in the Bruneau Lab. “But without Brahma, there was just a mass of inert cells. No beating at all.”
After further analysis, Bruneau’s team realized the reason the cells weren’t beating was because removing Brahma not only turned off genes required for heart cells, but also activated genes needed in brain cells. The heart precursor cells were now brain precursor cells.
The researchers then followed every step of differentiation, and unexpectedly discovered that these cells never returned to a pluripotent state. Instead, the cells took a far larger leap between stem cell paths than had ever been observed before.
“What we saw is that a cell in one valley of the Waddington landscape, with the right conditions, can jump into a different valley without first taking a lift back to the summit,” says Bruneau.
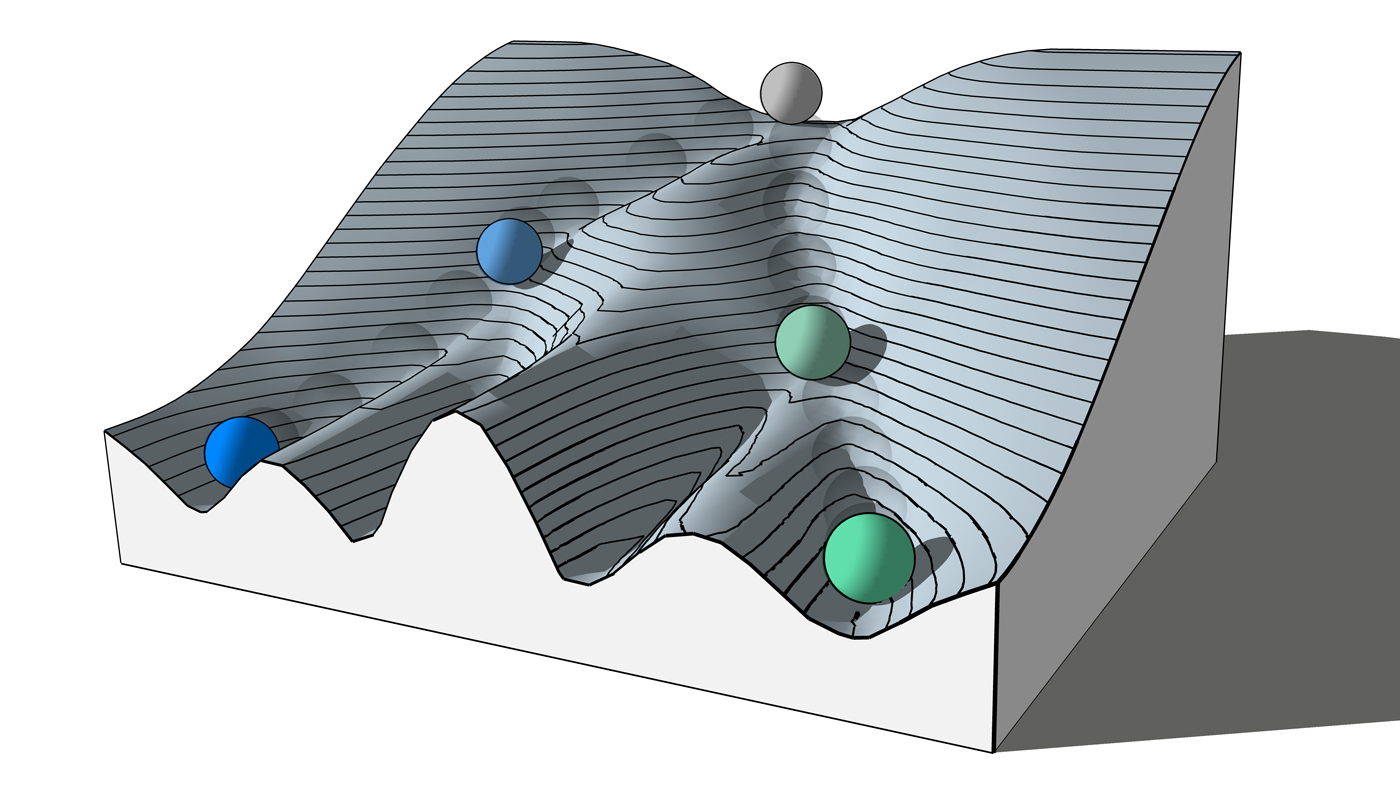
The Waddington landscape illustrates the path a stem cell (grey) takes to differentiate, or transform, into a precise type of cell (such as a heart or brain cell, shown here as blue or green). Gladstone researchers have now found that cells, with the right conditions, can jump into a different valley without first going back to the summit (for instance, jumping directly from the valley with blue cells to the one with green cells).
Lessons for Disease
While the environment of cells in a lab dish and in a whole embryo is quite different, the researchers’ observations hold lessons about cell health and disease. Mutations in the gene Brm have been associated with congenital heart disease and with syndromes that involve brain function. The gene is also involved in several cancers.
“If removing Brahma can turn mesoderm cells (like heart cell precursors) into ectoderm cells (like brain cell precursors) in the dish, then perhaps mutations in the gene Brm are what give some cancer cells the ability to massively alter their genetic program,” says Bruneau.
The findings are also important at a basic research level, he adds, as they can shed light on how cells might change their character in disease settings, such as heart failure, and for developing regenerative therapies, by inducing new heart cells for example.
“Our study also tells us that differentiation paths are far more intricate and fragile than what we thought,” says Bruneau. “A better knowledge of the paths of differentiation can also help us understand congenital heart—and other—defects, which arise in part through defective differentiation.”
For Media
Julie Langelier
Associate Director, Communications
415.734.5000
Email
About the Study
The paper “Brahma safeguards canalization of cardiac mesoderm differentiation” was published online by the journal Nature on January 26, 2022.
Other authors are Kavitha Rao, Andrew Blair, Kevin Hu, Reuben Thomas, Kevin So, Vasumathi Kameswaran, Jiewei Xu, Benjamin Polacco, Ravi Desai, Austin Hsu, Jonathon Muncie, Aaron Blotnick, Sarah Winchester, Leor Weinberger, Ruth Huttenhain, Irfan Kathiriya, and Nevan Krogan from Gladstone; Ali Khalilimeybodi and Jeffrey Saucerman from the University of Virginia; and Nilanjana Chatterjee from UCSF.
This work was supported by the National Institutes of Health (grants: P01HL089707, P01HL146366, UM1HL098179, R01HL114948, R01HL137755, 2T32- HL007731 26, C06 RR018928), the American Heart Association (grant 13POST17290043 and Career Development Award 861914), the Tobacco Related Disease Research Program (grant 22FT-0079), the Society for Pediatric Anesthesia, the Hellman Family Fund, a UCSF REAC Award, and the UCSF Department of Anesthesia and Perioperative Care.
About Gladstone Institutes
Gladstone Institutes is an independent, nonprofit life science research organization that uses visionary science and technology to overcome disease. Established in 1979, it is located in the epicenter of biomedical and technological innovation, in the Mission Bay neighborhood of San Francisco. Gladstone has created a research model that disrupts how science is done, funds big ideas, and attracts the brightest minds.
Support Discovery Science
Your gift to Gladstone will allow our researchers to pursue high-quality science, focus on disease, and train the next generation of scientific thought leaders.
New Tool Reveals the Secrets of HIV-Infected Cells
New Tool Reveals the Secrets of HIV-Infected Cells
Developed by Gladstone scientists, HIV-seq could uncover new opportunities for treating HIV.
News Release Research (Publication) HIV/AIDS Infectious Disease Roan LabVitamin B3 Therapy Offers Hope for Fatal Childhood Disease
Vitamin B3 Therapy Offers Hope for Fatal Childhood Disease
A new framework that matches vitamins with genetic diseases helped uncover that high-dose vitamin B3 can dramatically extend survival in mice with NAXD deficiency.
News Release Research (Publication) Rare Diseases Jain LabGladstone Scientist Nadia Roan Elected to American Academy of Microbiology
Gladstone Scientist Nadia Roan Elected to American Academy of Microbiology
Roan has made great strides in understanding how persistent viruses including HIV cause disease and how immunity to viruses shapes human health.
Awards News Release COVID-19 HIV/AIDS Infectious Disease Roan Lab