Gladstone NOW: The Campaign Join Us on the Journey✕
Yadong Huang and his team demonstrated in mice that the ApoE4 protein from neurons plays a much bigger disease-driving role in Alzheimer’s than previously thought.
Of all the known genetic risk factors for late-onset Alzheimer’s disease, the strongest is a gene for the protein called ApoE4. People with one copy of this gene are 3.5 times more likely, on average, to develop Alzheimer’s than others, and those with two copies face a 12-fold increased risk. However, exactly how ApoE4 boosts the risk of Alzheimer’s remains unclear.
Multiple types of cells in the brain make ApoE4—some of it is produced by neurons, but other brain cells called glia make it in higher quantities. For that reason, most prior research on this protein has focused on ApoE4 from glia.
Now, researchers at Gladstone Institutes are shining a brighter spotlight on ApoE4 produced by neurons. In a study published in the journal Nature Aging, they demonstrate in mice that ApoE4 from neurons plays a much bigger disease-driving role in Alzheimer’s than previously thought.
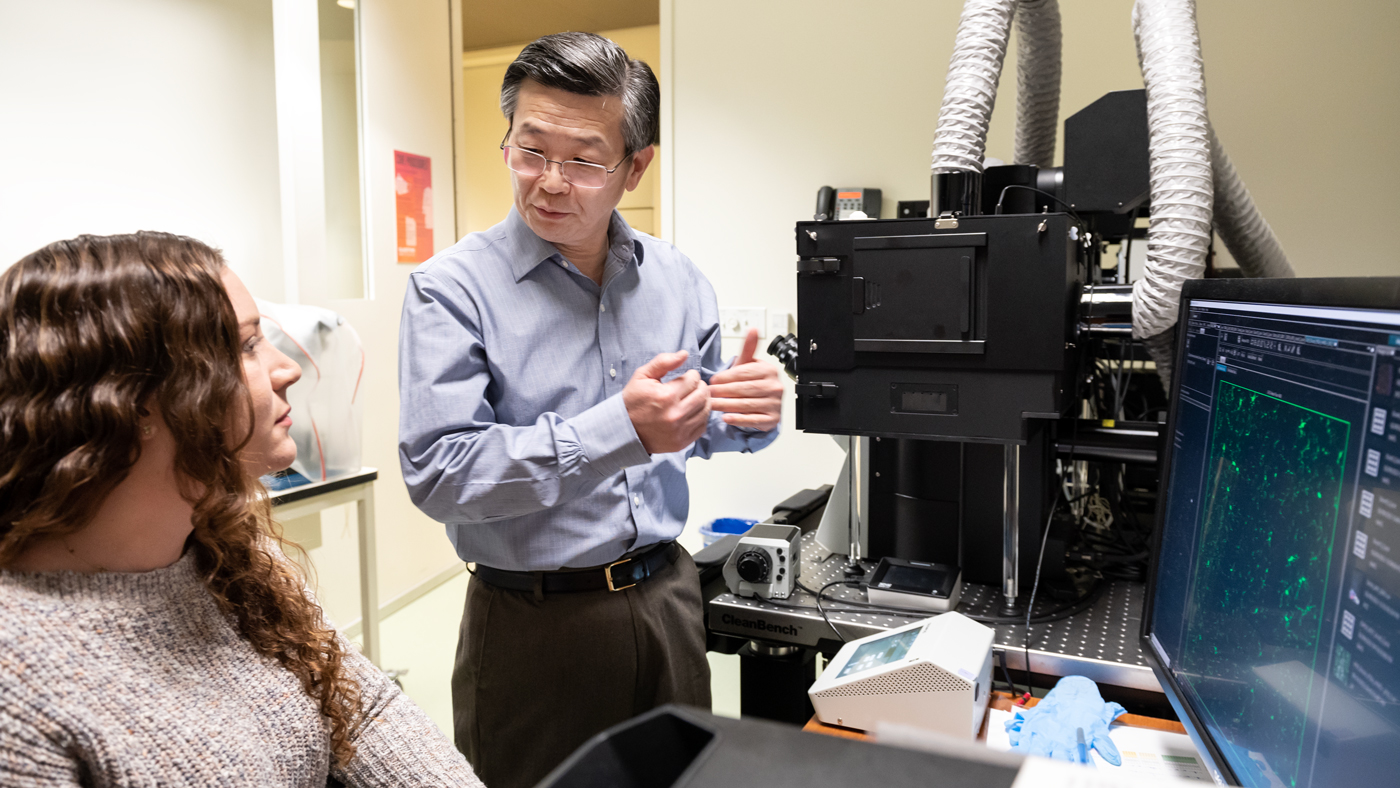
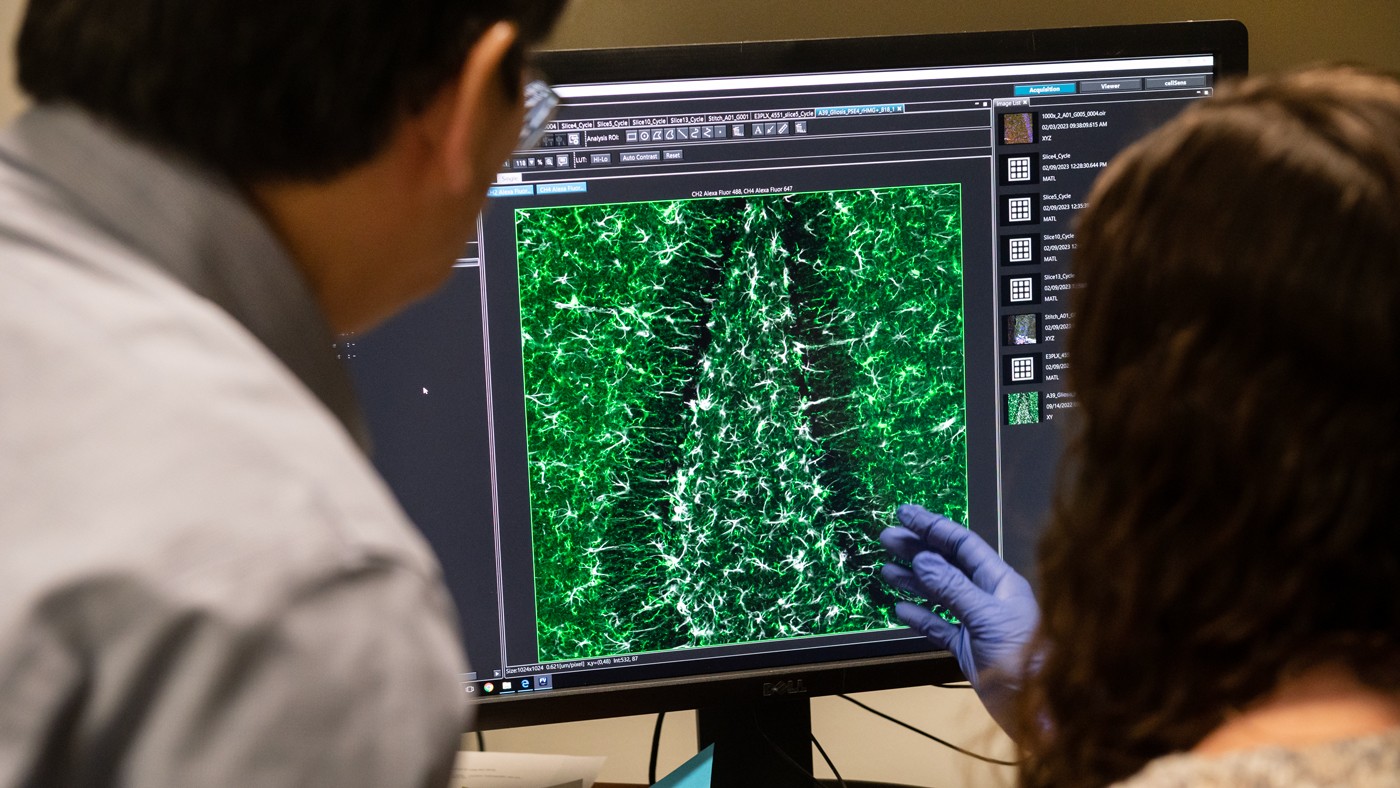
Huang (right) and his team, including Koutsodendris (left), created a mouse model for Alzheimer’s disease to study specifically the production of ApoE4 by neurons.
“This research could be a turning point in the field of ApoE research,” says Gladstone Senior Investigator Yadong Huang, MD, PhD, senior author of the study. “Our findings suggest an opportunity to explore new treatments that would specifically target neuronal ApoE4 to protect against Alzheimer’s disease.”
Deleting ApoE4 in Neurons to Reveal its Role
ApoE4 is actually one of three versions of the ApoE protein, which is found in every person’s body. Most people have the “healthy” version, ApoE3, while about 12 percent have the Alzheimer’s-protective version, ApoE2. But about 25 percent of North Americans have one copy of the gene for ApoE4, and up to 3 percent have two copies.
Most ApoE in our brains is produced by a type of glial cell called astrocytes, and previous research suggested that astrocytic ApoE4 contributes to Alzheimer’s disease. However, evidence from Huang and colleagues has hinted for several years that ApoE4 from neurons may play an even more important part.
“Under normal conditions, neurons don’t make much ApoE at all, but when under stress or in response to injury, they quickly increase production of this protein,” says Huang, who is also director of the Center for Translational Advancement at Gladstone, and professor of neurology and pathology at UC San Francisco (UCSF). “That’s why we are very interested in neuronal ApoE4 under disease conditions.”
“Our findings highlight the therapeutic potential of reducing neuronal ApoE4 in Alzheimer’s disease.”
To better understand the protein’s role, his team created a mouse model for Alzheimer’s disease in which the mouse ApoE gene was replaced by the human gene for ApoE4 or ApoE3. The mice also carry a unique form of the human tau protein that accumulates in the brain with aging—a hallmark of Alzheimer’s disease. Importantly, in the genetically engineered mice, ApoE production by neurons could be selectively eliminated, while preserving the production of ApoE by other cell types, allowing the scientists to examine exactly how deleting neuronal ApoE4 impacts disease progression in mice that mimic Alzheimer’s disease.
Striking Results of Protection
The scientists found that removing ApoE4 from neurons reduced many brain changes resembling Alzheimer’s disease.
In the models, deleting neuronal ApoE4 reduced the abnormal accumulation of tau by over 80 percent. It also protected against loss of neurons and shrinkage of the hippocampus, a part of the brain crucial for memory formation that degenerates in Alzheimer’s patients.
In addition, deleting neuronal ApoE4 protected against loss of myelin sheaths—insulating layers that shield neurons and help their electrical signals travel faster. It reduced overexcitation of neurons, which often occurs in Alzheimer’s disease, and it decreased the abnormally intense reactions of glial cells—key contributors to degeneration—commonly seen in the disease.

Koutsodendris (right), a former trainee in Huang's (left) lab, helped show that removing ApoE4 produced by neurons—even though it only accounts for a small portion of this protein in the brain—leads to significant reductions in the pathology of Alzheimer's disease.
“These extensive reductions in pathology were striking, especially since neuronal ApoE4 only accounts for a small portion of the ApoE produced in the brain,” says Nicole Koutsodendris, PhD, lead author of the study, and former graduate student in Huang’s lab at Gladstone and in the Developmental and Stem Cell Biology program at UCSF.
“Our results strongly suggest that neuronal ApoE4 is critical for the development of Alzheimer’s disease in ApoE4 carriers,” Huang says.
A New Direction for Drug Development
While some medications and other treatments may slow the progression of Alzheimer’s disease or help treat symptoms, no cure exists yet. And patients are in urgent need of solutions.
By establishing a key role of neuronal ApoE4, Huang’s team opens up new possibilities for the treatment of Alzheimer’s disease. For instance, drugs or gene-editing strategies could be developed to block mechanisms responsible for the production of ApoE4 within neurons.
“Our findings highlight the therapeutic potential of reducing neuronal ApoE4 in Alzheimer’s disease,” says Huang. “They open up exciting new opportunities for the development of better drugs or strategies to treat this devastating disease.”
For Media
Julie Langelier
Associate Director, Communications
415.734.5000
Email
About the Study
The paper “Neuronal APOE4 Removal Protects Against Tau-Mediated Gliosis, Neurodegeneration, and Myelin Deficits” was published in the journal Nature Aging on February 20, 2023.
Other authors on the study include Jessica Blumenfeld, Ayushi Agrawal, Michela Traglia, Brian Grone, Misha Zilberter, Oscar Yip, Antara Rao, Maxine R. Nelson, Yanxia Hao, Reuben Thomas, Seo Yeon Yoon, and Patrick Arriola from Gladstone.
This study was funded in part by the National Institute on Aging (R01AG071697, P01AG073082, R01AG061150, F31AG074672, and F31AG074690).
About Gladstone Institutes
Gladstone Institutes is an independent, nonprofit life science research organization that uses visionary science and technology to overcome disease. Established in 1979, it is located in the epicenter of biomedical and technological innovation, in the Mission Bay neighborhood of San Francisco. Gladstone has created a research model that disrupts how science is done, funds big ideas, and attracts the brightest minds.
Featured Experts
Support Discovery Science
Your gift to Gladstone will allow our researchers to pursue high-quality science, focus on disease, and train the next generation of scientific thought leaders.
Disrupted Boundary Between Cell Types Linked to Common Heart Defects
Disrupted Boundary Between Cell Types Linked to Common Heart Defects
Gladstone scientists identified a cellular boundary that guides heart development and revealed how disrupting it can lead to holes in the heart’s wall.
News Release Research (Publication) Congenital Heart Disease Cardiovascular Disease Bruneau LabGene Editing Strategy Could Treat Hundreds of Inherited Diseases More Effectively
Gene Editing Strategy Could Treat Hundreds of Inherited Diseases More Effectively
Scientists at Gladstone show the new method could treat the majority of patients with Charcot-Marie-Tooth disease.
News Release Research (Publication) Neurological Disease Conklin Lab CRISPR/Gene EditingGenomic Maps Untangle the Complex Roots of Disease
Genomic Maps Untangle the Complex Roots of Disease
Findings of the new study in Nature could streamline scientific discovery and accelerate drug development.
News Release Research (Publication) Marson Lab Genomics Genomic Immunology




