Gladstone NOW: The Campaign Join Us on the Journey✕

Gladstone researchers, including Ken Nakamura (left), Zak Doric (center), and Huihui Li (right), tracked mitochondria inside neurons and uncovered a new recycling pathway that may be linked to Parkinson's disease.
Scientists have long known that living cells are master recyclers, constantly breaking down old parts and building them back up into new molecular machines. Now, researchers at Gladstone Institutes have taken a closer look at the life cycle of energy-generating cellular power plants—called mitochondria— inside brain cells, and how they might be recycled. They showed that genes associated with Parkinson’s disease play key roles in this process.
“This work gives us unprecedented insight into mitochondria’s life cycle and how they are recycled by key proteins that, when mutated, cause Parkinson’s disease,” says Gladstone Associate Investigator Ken Nakamura, MD, PhD, senior author of the new study. “It suggests that mitochondrial recycling is critical to maintaining healthy mitochondria, and disruptions to this process can contribute to neurodegeneration.”
Breaking Down Damaged Mitochondria
In most cells, damaged mitochondria are decomposed in a process known as mitophagy, which is initiated by two proteins, PINK1 and Parkin. Mutations in these same proteins also cause hereditary forms of Parkinson’s disease. While the role of PINK1 and Parkin in mitophagy has been heavily studied in many cell types, it has been unclear whether these proteins act the same way in neurons—the type of brain cells that die in Parkinson’s disease. Indeed, neurons have unusually high energy needs and their mitochondria are much more resistant to degradation by Parkin than those in other cell types.
In the new study published in the journal Science Advances, Nakamura’s group followed mitochondria inside living neurons and examined how PINK1 and Parkin affected their fate.
But mitochondria are small and they move inside cells, frequently fusing with each other or splitting in two, which makes them difficult to track.
“We had to develop a new way of tracking individual mitochondria over long periods of time, almost a full day,” says Zak Doric, a graduate student at Gladstone and UC San Francisco (UCSF) and co-first author of the new study. “Getting that technique up and running was quite a challenge.”
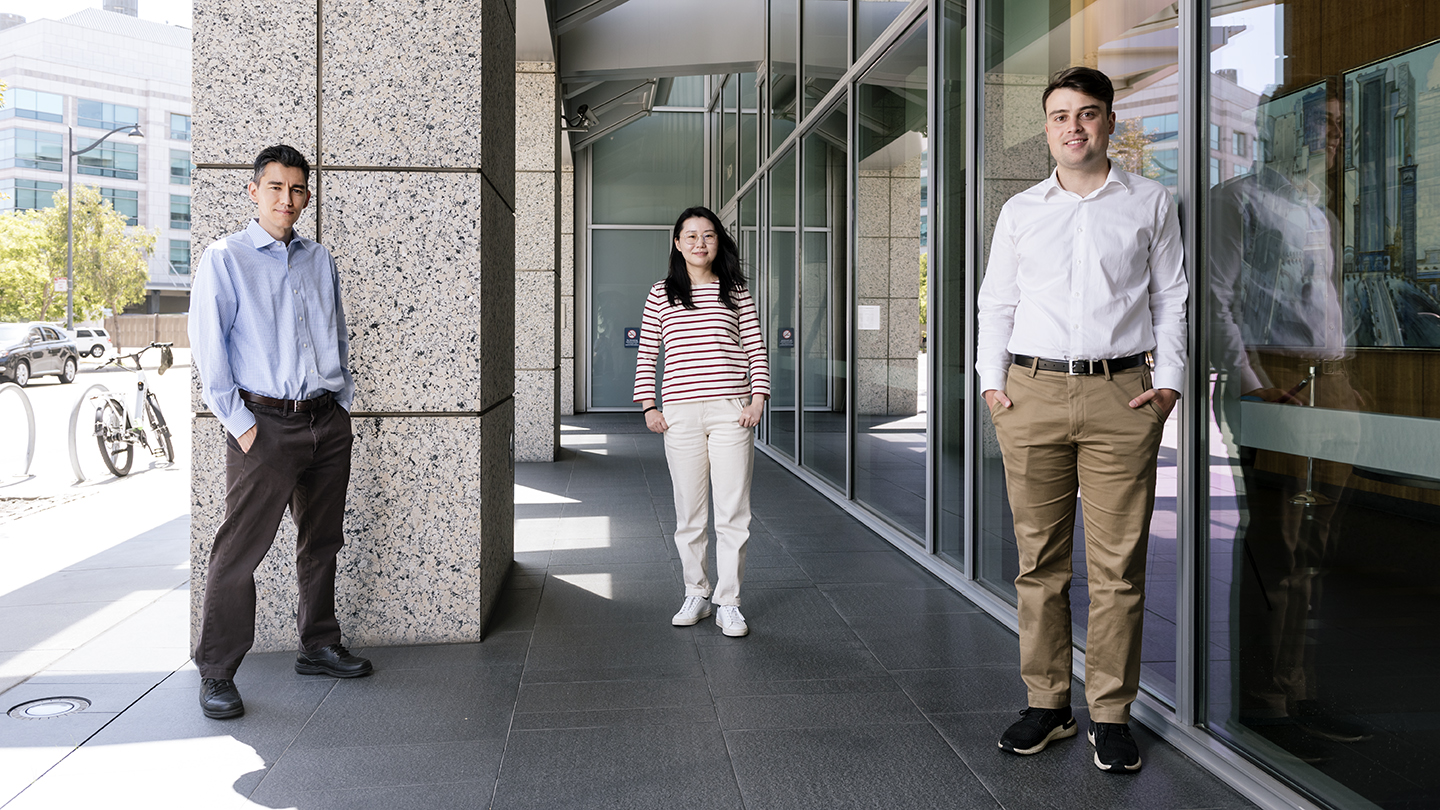
Ken Nakamura (left), Huihui Li (center), and Zak Doric (right) identified a process involving mitochondria that may be critical in protecting against neurodegeneration in Parkinson’s disease.
The scientists also used a method that allowed them to generate larger-than-normal mitochondria, making them easier to see under a microscope.
They found that Parkin proteins encircled damaged mitochondria and targeted them for degradation, demonstrating that mitophagy starts in neurons in the same way as in other cell types. But thanks to their new approach, they could watch the process unfold in great detail. For instance, they documented the key initial steps in which damaged, Parkin-coated mitochondria fuse with other components inside the cell to form mitochondria-degrading structures called mitolysosomes.
“We were able to visualize these steps at a level that hasn’t been done before in any cell type,” says Nakamura, who is also an associate professor of neurology at UCSF.
The high resolution of their approach will allow them to understand with great precision how Parkin and PINK1 affect mitochondrial degradation in Parkinson’s disease.
A New Kind of Recycling
The researchers then examined the later phases of mitophagy, monitoring what happens to mitochondria in the mitolysosomes.
“Until now, nobody has known what happens next to these mitolysosomes,” says Nakamura.
So far, scientists had assumed that mitolysosomes rapidly break down into molecules that the cell can reuse to build new mitochondria from scratch. Nakamura and his team showed that, instead, the mitolysosomes survived for hours inside cells. Remarkably, and unexpectedly, some mitolysosomes were engulfed by healthy mitochondria, while other times, they suddenly burst, releasing their contents into the interior of the cell, including some proteins that were still functional.
“This appears to be a new mitochondrial quality control, recycling system,” says Huihui Li, PhD, a Gladstone postdoctoral scholar and co-first author of the new paper. “We think we’ve uncovered a pathway of mitochondrial recycling—which is like salvaging valuable furniture in a house before demolishing it.”
Importantly, the study shows that the recycling pathway identified by the scientists requires PINK1 and Parkin, supporting that mitochondrial recycling may also be critical in protecting against neurodegeneration in Parkinson’s disease.
“Dopamine neurons that die in Parkinson’s disease are particularly susceptible to mutations in PINK1 and Parkin,” says Nakamura. “Our study advances our understanding of how these two key Parkinson’s disease proteins degrade and recycle mitochondria. Our future studies will investigate how these pathways contribute to disease and how they can be targeted therapeutically.”
For Media
Julie Langelier
Associate Director, Communications
415.734.5000
Email
About the Study
The paper “Longitudinal Tracking of Neuronal Mitochondria Delineates PINK1/Parkin-Dependent Mechanisms of Mitochondrial Recycling and Degredation” was published by the journal Science Advances on August 6, 2021.
Other authors are: Amandine Berthet, Mai Nguyen, Julia Margulis, Rebecca Fang, and Steve Finkbeiner of Gladstone; Danielle Jorgens of UC Berkeley; Ivy Hsieh, Jayanta Debnath, and Eric Huang of UC San Francisco; and Hiromi Sesaki of Johns Hopkins.
The work at Gladstone was supported by the Joan and David Traitel Family Trust, the Betty Brown Family, a Career Awards for Medical Scientists from the Burroughs-Wellcome Fund, the National Institutes of Health (RO1NS091902, 5P30 NS069496), the Hillblom Foundation, and a Berkelhammer Award for Excellence in Neuroscience.
About Gladstone Institutes
Gladstone Institutes is an independent, nonprofit life science research organization that uses visionary science and technology to overcome disease. Established in 1979, it is located in the epicenter of biomedical and technological innovation, in the Mission Bay neighborhood of San Francisco. Gladstone has created a research model that disrupts how science is done, funds big ideas, and attracts the brightest minds.
Featured Experts
Support Discovery Science
Your gift to Gladstone will allow our researchers to pursue high-quality science, focus on disease, and train the next generation of scientific thought leaders.
New Tool Reveals the Secrets of HIV-Infected Cells
New Tool Reveals the Secrets of HIV-Infected Cells
Developed by Gladstone scientists, HIV-seq could uncover new opportunities for treating HIV.
News Release Research (Publication) HIV/AIDS Infectious Disease Roan LabVitamin B3 Therapy Offers Hope for Fatal Childhood Disease
Vitamin B3 Therapy Offers Hope for Fatal Childhood Disease
A new framework that matches vitamins with genetic diseases helped uncover that high-dose vitamin B3 can dramatically extend survival in mice with NAXD deficiency.
News Release Research (Publication) Rare Diseases Jain LabGladstone Scientist Nadia Roan Elected to American Academy of Microbiology
Gladstone Scientist Nadia Roan Elected to American Academy of Microbiology
Roan has made great strides in understanding how persistent viruses including HIV cause disease and how immunity to viruses shapes human health.
Awards News Release COVID-19 HIV/AIDS Infectious Disease Roan Lab