Gladstone NOW: The Campaign Join Us on the Journey✕
Building on Shinya Yamanaka’s human induced pluripotent stem cells, Gladstone investigators are developing creative strategies to use stem cells toward understanding and treating diseases.
In December 2012, Shinya Yamanaka, MD, PhD—a senior investigator at Gladstone Institutes—stepped onto the stage at the Karolinska Institute in Sweden and accepted the Nobel Prize in Medicine. Yamanaka, a few years earlier, had discovered a way to convert run-of-the-mill skin cells into stem cells that had the potential to become any cell in the body. In his Nobel lecture, Yamanaka listed the ways that he foresaw these induced pluripotent stem cells, or iPS cells, changing biomedical research and medicine. “The history of iPS cell research has only just begun,” he said, “and this technology has a remarkable potential for use in cell therapy, drug screening, and personalized medicine.”
Today, scientists at Gladstone and around the world are already fulfilling that prediction. Researchers have created thousands of iPS cell lines, discovered ways to coax those cells into a myriad of tissue types, used them as a tool to study disease, and even begun creating therapies using the stem cells.
“This technology has allowed us to make human tissues that were inaccessible before,” says Gladstone President Deepak Srivastava, MD. “We don’t have easy access to someone’s heart or brain, but we do have easy access to their skin or blood cells.”
The idea that iPS cells can create new tissues or help the body regenerate damaged cells has raised hopes for eventual iPS cell–based therapeutics.
But the game-changing technology is still riddled with challenges and research scientists are cautious about overhyping its potential. It can be a struggle to get consistent results between batches of stem cells, and applying results from the lab to patients is slow going.
“There’s still a long way to go in this field,” says Sheng Ding, PhD, a senior investigator at Gladstone. “We see a very bright horizon off in the future, but we’re still really at the starting line.”
Limitless Source of Cells
The cells found nestled on the inside of a days-old human embryo are the tabula rasa of cells; they will eventually divide and differentiate to form every tissue in the human body. Removed from an embryo, these embryonic stem cells are still pluripotent— they can continuously self-replicate but also be coaxed to give rise to all the other cells types. For years, researchers assumed this was a one-way path, and once an embryonic stem cell had differentiated into a cell—whether a heart, brain, or skin cell— it could never return to the more juvenile stem cell state. It was thought that the only way to study stem cells, or use them to generate adult tissues, was to harvest them from embryos. Yamanaka, though, proved otherwise.
Yamanaka’s group added four key genes to fibroblasts, turning back their developmental clock and producing iPS cells from these ordinary skin cells. Research using embryonic stem cells had been limited by legal and ethical conundrums, but with iPS cells, scientists suddenly had a limitless source of stem cells.
As much as Yamanaka’s exact techniques were useful, the very idea that adult cells could have their slates wiped clean was transformational. Over the handful of years after Yamanaka’s initial discovery, Gladstone researchers were among those to develop new protocols to generate iPS cells. Ding, for instance, discovered that with the right cocktail of specially engineered proteins or small molecules, he could create iPS cells without ever introducing genes into cells.
The power in iPS cells, of course, resides largely in what they can become—heart or muscle or liver or brain or any number of other human tissues. Researchers have pioneered methods to coax iPS cells down each of these paths or, in some cases, discovered how to directly convert one adult cell type into another, skipping the iPS cell stage entirely.
Take just one cell type—the cardiomyocyte muscle cells that make the heart beat. Srivastava pinpointed a combination of three genes that turned cardiac scar-forming cells into cardiomyocytes right where they are, restoring heart function in animals after damage. In collaboration with Ding, the researchers then developed a second method, using small molecules—rather than genes—to transform support cells into cardiomyocytes. Separately, Srivastava and Gladstone Senior Investigator Bruce Conklin, MD uncovered the role of microRNA molecules in regulating the fate of pluripotent stem cells. In each case, the introduced molecules use different mechanisms to turn up or down the regulation of dozens of other genes and pathways.
“These methods all have their advantages as well as their disadvantages,” says Ding. “I wouldn’t say any is necessarily better for all purposes.”
Disease in a Dish
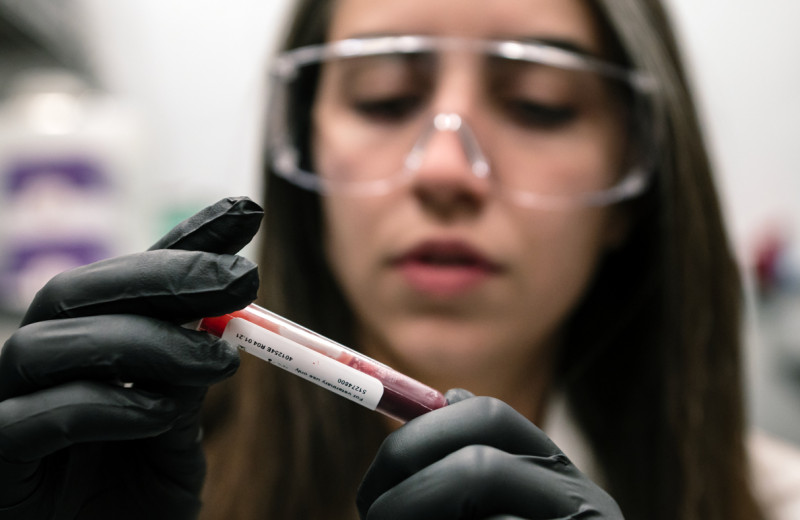
If you start with fibroblasts from a healthy human, convert them into iPS cells, and then generate brain cells, you’ll end up with relatively normal, healthy brain cells. But if you start with skin cells from a person with a genetic disease, the cells you produce in the end may not be normal—and for researchers, that’s a good thing. It means iPS cells can be used to study disease.
In his lab at Gladstone, Senior Investigator and Director Steve Finkbeiner, MD, PhD has access to more than 2,000 iPS cell lines that he’s collected from patients with neurodegenerative diseases—Alzheimer’s, Parkinson’s, ALS, Huntington’s, and a handful of others. From each culture, he and his colleagues can create brain cells and study exactly what makes the cells different from brain cells in healthy individuals.
“In part, it’s an effort to get a handle on the variability seen in these diseases,” says Finkbeiner. “If we see something in one iPS line, does it appear across lines from many different patients?” The answer to this question is key to successful clinical trials and achieving the goals of precision medicine.
When Finkbeiner’s group finds a molecular pathway that’s gone awry in one patient’s diseased brain cells, he can not only test whether that pathway is dysfunctional in other patients, he can also use the cells to screen drugs for their ability to correct the underlying pathophysiology. Earlier this year, Finkbeiner and collaborators around the country published the results of a study on iPS cells derived from patients with Huntington’s disease. The cells helped them discover not only that brain cells affected by Huntington’s have decreased levels of the molecular energy currency ATP, but how to use small molecules to increase those ATP levels to normal.

Huang (left), Ding (center), and Srivastava (right) have developed novel ways of reprogramming adult cells into pluripotent stem cells, using cocktails of chemicals or different genes than Yamanaka’s original set.
Similar stories abound. Conklin used iPS cells derived from patients with a rare genetic disease called fibrodysplasia ossificans progressiva to reveal the role that certain blood vessel cells play in the disease. Recently, he’s used those same cells to screen drugs for their ability to fix the molecular blunder and pinpointed one compound that helps treat the disease in mice.
“The idea with all these diseases in a dish is that you can first study the underlying molecular pathophysiology and then use it as a drug-discovery, or drug-screening, or drug-testing device,” says Conklin.
While similar studies could already be done using mouse cells, some genetic mutations have different effects in mice and humans. Validating results from mice in human cells can help confirm the importance of molecular pathways or drug targets in humans before clinical trials, says Gladstone Senior Investigator Yadong Huang, MD, PhD.
Recently, Huang and his colleagues generated iPS cells from people with the ApoE4 genetic variant—a version of the ApoE gene that greatly increases one’s chance of developing Alzheimer’s disease. When the researchers made neurons from these iPS cells, they were able to show that the ApoE4-carrying cells had higher levels of tau phosphorylation, as well as increased production of amyloid-beta, two hallmarks of Alzheimer’s in the brain. The same hadn’t been seen in mouse cells. Moreover, the team went on to test an ApoE4-targeting drug candidate in the same human iPS-derived neurons and showed that it could correct the defects.
Two Disruptive Technologies Come Together
In 2012, a few months before Yamanaka’s Nobel Prize, Jennifer Doudna, PhD—now a senior investigator at Gladstone—discovered how to use the bacterial system called CRISPR to efficiently edit the DNA inside living cells. The molecular scissors upended numerous fields of biology; they allow researchers to introduce specific genetic mutations into cells, or repair existing genetic mutations.
The advent of CRISPR was timely for researchers working with iPS cells. Most previous gene-editing approaches didn’t work well with stem cells, but CRISPR offered a way to control not only the fate of iPS cells, but the gene sequences inside those cells.
“These are two incredibly disruptive technologies which work very well together,” says Conklin.
Before CRISPR, Conklin says that it was hard to prove, without the shadow of a doubt, the link between a gene mutation and a molecular pathway in hard-to-access human tissues like the brain and heart. When CRISPR debuted, that changed.
“Essentially, the entire world of human genetics opened up to us in a way that just wasn’t available before,” he says.

Conklin (left), McDevitt (right), and Finkbeiner (not shown) combine hiPS cell technology and CRISPR genome manipulations to study or edit genetic factors that play crucial roles in disease or in normal tissue formation.
Early in the days of iPS cells, Conklin’s lab cultured a line of stem cells from a healthy person’s fibroblast skin cells. Now known as “wild type C” or WTC, the cells have been used in countless experiments as a workhorse cell line around the world—Conklin says they’re “the model for a human”—and, in Conklin’s lab, mutated dozens of times into new lines of cells using CRISPR.
With Srivastava, Conklin used CRISPR to add or correct heart disease–related gene mutations in human iPS cells. By generating cardiomyocytes from those cells, the researchers were able to study the exact molecular effect of the mutations in heart cells. Srivastava and Conklin are continuing to combine CRISPR and iPS cell technology to screen the effects of thousands of other genetic mutations on heart development and disease.
CRISPR is also becoming a tool for iPS cell generation itself—Ding has successfully used CRISPR-based technology to reprogram fibroblasts into iPS cells not by directly editing genes, but instead by turning on the right combination of genes. He says that this may represent a safer method for human iPS cell generation.
As researchers improve methods to produce iPS cells and send them down developmental pathways, they’ve also set their sights on making more complex tissues from stem cells—most organs contain more than one cell type, organized into distinct patterns. Being able to generate these kinds of cellular architectures in the lab would be a step toward building organs. But basic questions remain about how stem cells, in a developing embryo, form these initial patterns.
To help shed light on that developmental process, Senior Investigator Todd McDevitt, PhD recently applied CRISPR to disrupt various genes in a subset of iPS cells in a culture. By only applying the technology to some cells in each mixture, he could study how the cells formed patterns as their populations diverged—a phenomenon known as “breaking symmetry”. McDevitt’s group has now used computer analysis and simulation programs to analyze the results of many such experiments—with each revealing roles of different genes in the physical organization of the cells. The program has started to successfully predict exactly how cells in a culture will morph when symmetry is broken in different ways and at different times.
“If we understand what influences the organization of cells, then we can start to move toward controlling that organization inside complex multicellular systems,” says McDevitt.
Moving In Vivo
The ultimate promise of stem cells is that they offer a way to cure disease—replacing neurons damaged in neurodegenerative diseases, offering a new source of insulin for diabetics, or healing the tissue that’s hurt in a heart attack, for example. Clinical trials that implant iPS-derived cells into the human body have begun and are increasing rapidly. But it will take many years of rigorous and careful study before such approaches become approved therapies.
“There’s this misperception among some people that stem cells are some sort of instant elixir; that you can inject them into your body and see immediate medical improvements,” says Finkbeiner. “That’s not the case. Clinics promoting so-called ‘stem cells’ as this kind of magic bullet aren’t backed up by real research,” he adds. “Most of these clinics are based in no science at all, do not use pluripotent stem cells, and actually can do more harm than good.”
Researchers studying how to use iPS cells and iPS cell–derived tissues in the body are, for the most part, still focused on making the technology work in mice and large animals. Huang, for instance, uses iPS cells to generate inhibitory neurons—a type of brain cell that’s dysregulated in Alzheimer’s disease. When he implants the new neurons into the brains of mice carrying the Alzheimer’s-associated gene ApoE4, their memory improves. But he still has a laundry list of tests to run before such a therapy is used in humans. “This needs time; the public needs to be patient with us,” he says. He’s talking not just about his own research, but the stem cell field in general.
And there are countless ways that iPS cells—or tissues derived from iPS cells—are slowly offering new therapeutic possibilities. Using iPS cells as a tool to discover new drugs, and predict what will work to treat disease—whether a small molecule drug or a CRISPR approach—is perhaps the lowest hanging fruit, Finkbeiner says. But there are other possibilities.

Thanks to their close connection to Gladstone Senior Investigator Shinya Yamanaka (center), Gladstone researchers have been at the forefront of hiPS cell technology development and applications.
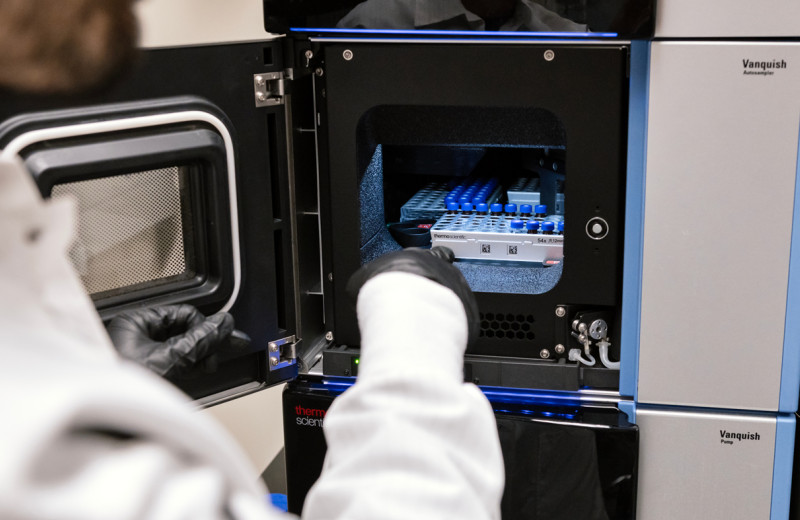
McDevitt, for example, is experimenting with ways to mimic the effect of stem cells without actually transplanting cells into people’s bodies. Scientists knew that when you transplant stem cells into an animal, some of their restorative approach is due not only to the cells themselves, but to compounds that the cells release. McDevitt’s group is trying to narrow down what those healing compounds are. They’ve engineered a new high-density stem cell culture system that can generate a concentrated form of the cellular products. Then, they chemically characterize the compounds in the liquid media surrounding the stem cells.
“It’s complex; there are a lot of things that cells secrete or produce,” says McDevitt. “But we want to be able to control that so it’s the same every time.”
He and his colleagues have recently focused on how the secretions from iPS cell cultures can rejuvenate hematopoietic stem cells (HSCs)—which form blood and immune cells—from older individuals. Typically, older HSCs don’t self-renew as often as younger cells, and produce a different balance of new cells. It may, in part, explain why older humans are more likely to get sick with illnesses like influenza. When McDevitt added secretions from iPS cells to these older cells however, they began to resemble HSCs seen in younger people. His group continues to probe exactly what compounds are responsible, and what their effect on various other tissue types is.
At Gladstone, it’s easy to get caught up in the excitement of iPS cell research. The technical know-how that emerged, thanks to Yamanaka’s role at Gladstone, allowed its researchers to master the challenges of iPS cell research early on. And as the field matures, Gladstone researchers remain at the forefront, pushing the boundaries of how iPS cells can be used to study and treat disease.
“We’ve been an epicenter for studying human iPS cells and manipulating their genomes,” says Srivastava. “Integrating that with our deep knowledge and interest in human disease has given us a really unique program.”
Support Discovery Science
Your gift to Gladstone will allow our researchers to pursue high-quality science, focus on disease, and train the next generation of scientific thought leaders.
New Tool Reveals the Secrets of HIV-Infected Cells
New Tool Reveals the Secrets of HIV-Infected Cells
Developed by Gladstone scientists, HIV-seq could uncover new opportunities for treating HIV.
News Release Research (Publication) HIV/AIDS Infectious Disease Roan LabVitamin B3 Therapy Offers Hope for Fatal Childhood Disease
Vitamin B3 Therapy Offers Hope for Fatal Childhood Disease
A new framework that matches vitamins with genetic diseases helped uncover that high-dose vitamin B3 can dramatically extend survival in mice with NAXD deficiency.
News Release Research (Publication) Rare Diseases Jain LabRed Blood Cells Soak Up Sugar at High Altitude, Protecting Against Diabetes
Red Blood Cells Soak Up Sugar at High Altitude, Protecting Against Diabetes
New study shows red blood cells act as hidden glucose sponges in low-oxygen conditions, explaining why people living at high altitude have lower diabetes rates and pointing toward new treatments.
News Release Research (Publication) Diabetes Jain Lab