Gladstone NOW: The Campaign Join Us on the Journey✕
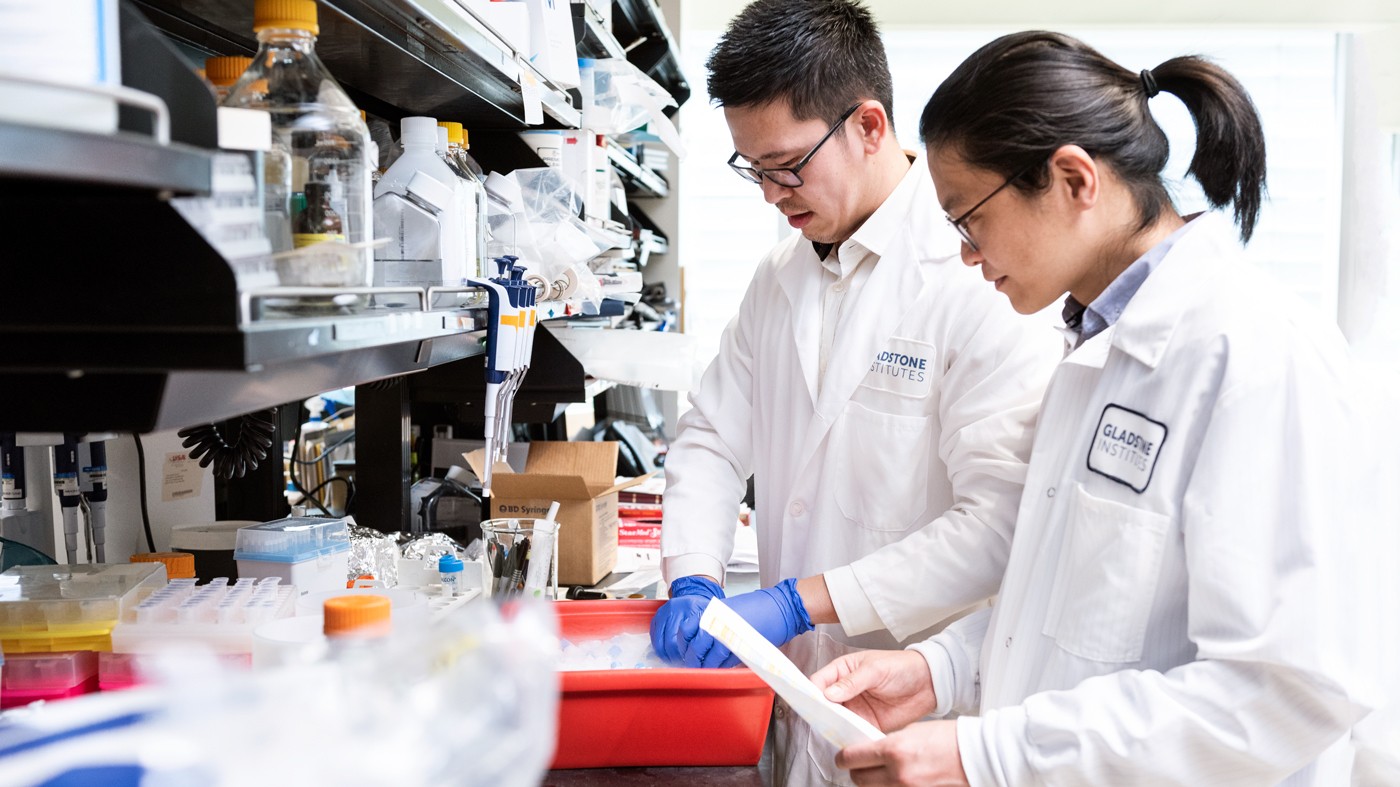
Scientists in Lennart Mucke's lab at Gladstone report new findings that could guide the development of better therapeutic strategies for Dravet syndrome and related conditions. Shown here are the study's first authors, Eric Shao (left) and Che-Wei Chang (right).
Children with Dravet syndrome, a severe form of epilepsy that begins in infancy, experience seizures, usually for their entire life. They are at high risk of sudden unexpected death in epilepsy (SUDEP) and can also develop intellectual disability and autism. Available treatments typically fail to improve these symptoms.
Now, a group of scientists at Gladstone Institutes led by Lennart Mucke, MD, reports new findings in the journal Science Translational Medicine that could guide the development of better therapeutic strategies for Dravet syndrome and related conditions.
The researchers previously discovered, in a mouse model of Dravet syndrome, that genetically removing the protein tau from the entire body during embryonic development reduces epilepsy, SUDEP, and autism-like behaviors. In the new study, they pinpoint the key cell type in the brain in which tau levels must be reduced to avoid these problems. They also show that lowering tau is still effective in mice when the intervention is delayed until after their birth.
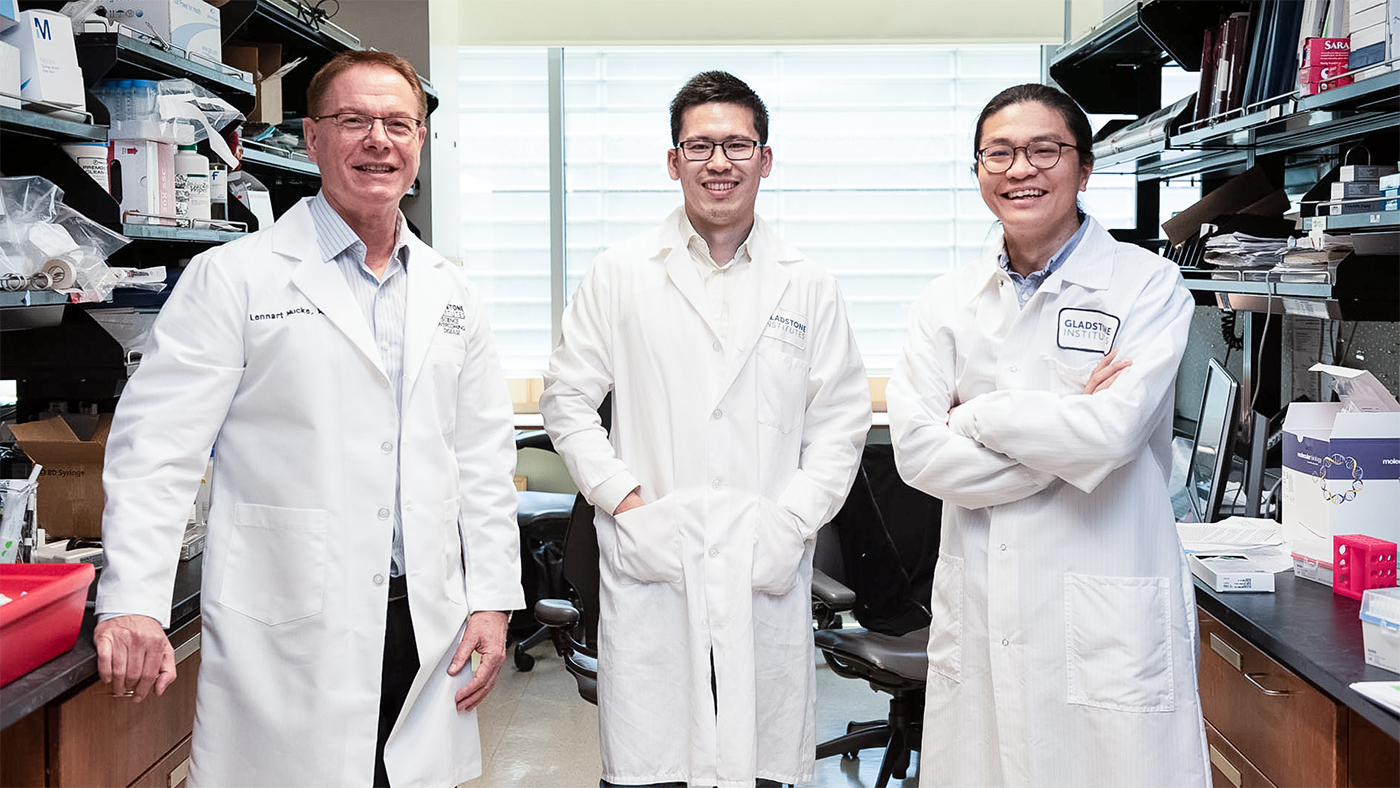
A team of scientists led by Mucke (left), and including Eric Shao (center) and Che-Wei Chang (right), discovered a promising treatment strategy targeting the protein tau that could be useful for Dravet syndrome, as well as epilepsy, autism, and Alzheimer's disease.
“Our findings provide new insights into the cellular mechanisms by which tau reduction prevents abnormal overexcitation in the brain,” says Mucke, director of the Gladstone Institute of Neurological Disease. “They are also encouraging from a therapeutic perspective, since in humans, initiating treatment after birth is still more feasible than treating embryos in the womb.”
Tau is a promising therapeutic target not only for Dravet syndrome, but also for a variety of other conditions, including different types of epilepsy and some forms of autism, as well as Alzheimer’s disease and related neurodegenerative disorders.
Pinpointing the Crucial Brain Cells
A well-functioning brain depends on the correct balance between the activity of excitatory and inhibitory neurons—the former stimulate the activity of other neurons, while the latter suppress it. Dravet syndrome causes an imbalance between these types of cells, resulting in abnormally high and synchronized activity in brain networks that can manifest as seizures and other symptoms.
Mucke and his colleagues recently showed that removing tau from the entire brain changes the activities of both excitatory and inhibitory neurons, although in different ways. The current study aimed to determine whether it is more important to reduce tau in excitatory or inhibitory neurons.
For this purpose, the scientists used genetic tools to eliminate tau selectively from one or the other cell type in the Dravet mouse model. They found that removing tau from excitatory neurons reduced disease manifestations, whereas removing tau from inhibitory neurons did not.
“This means that tau production in excitatory neurons sets the stage for all these abnormalities to occur, including autistic behaviors, epilepsy, and sudden unexpected death,” says Mucke, who is also the Joseph B. Martin Distinguished Professor of Neuroscience and a professor of neurology at UC San Francisco.
Initiating Treatment after Birth
While the genetic approaches the scientists used to remove tau from specific cell types are effective and precise, they are not yet easy to use as a therapeutic intervention in humans. So, the team turned to a more practical option: global tau reduction in the brain with DNA fragments known as antisense oligonucleotides, or ASOs. The scientists delivered an anti-tau ASO into the brain of mice 10 days after birth and found that most symptoms of Dravet syndrome were gone 4 months later.
“We observed a robust reduction of SUDEP, seizure activity, and repetitive behaviors,” says Eric Shao, PhD, a scientist in Mucke’s lab and first author of the study.
In addition, the ASO treatment had no obvious side effects.
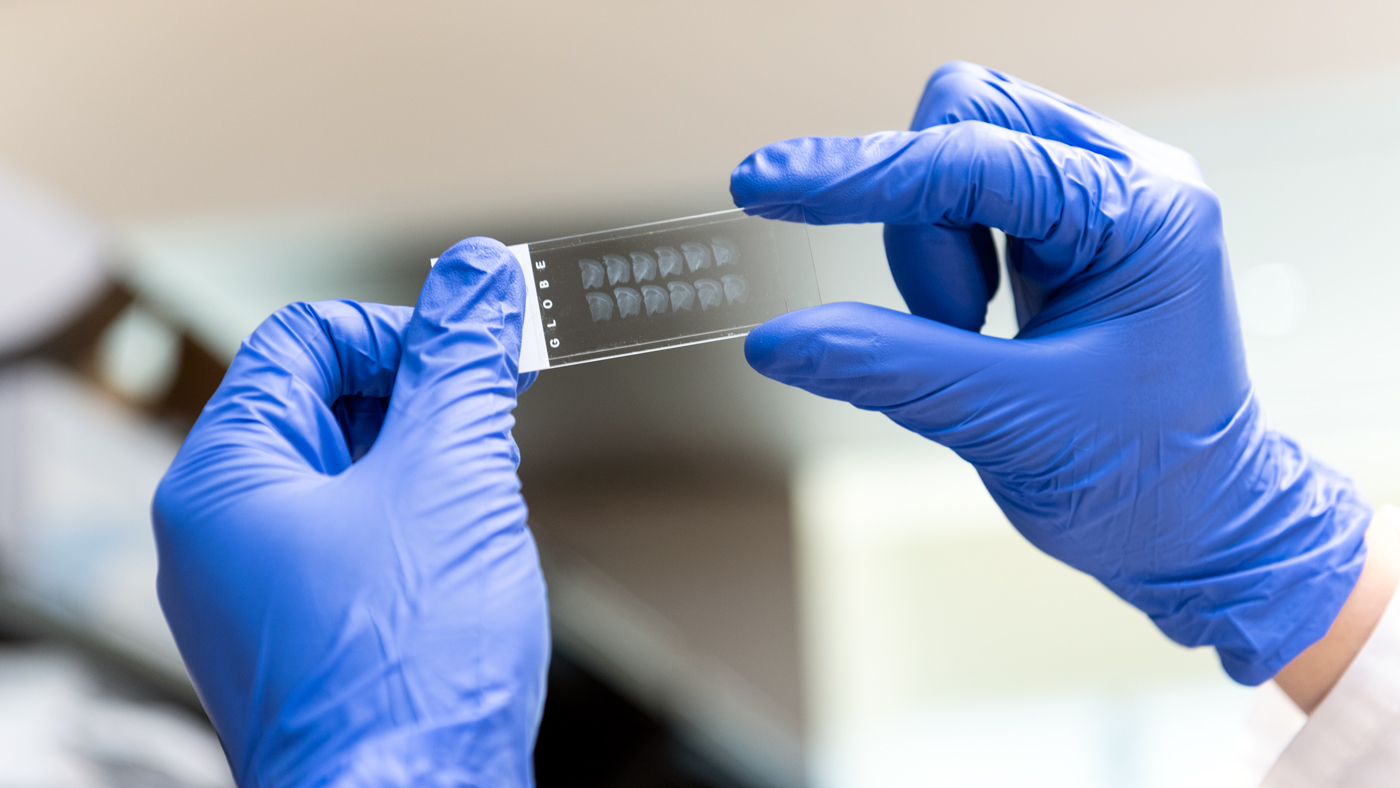
Gladstone scientists found that globally reducing tau in the brain with an ASO reduced most symptoms of Dravet syndrome. Here, Shao looks at sections of the mouse brain to determine whether the anti-tau ASO penetrated all regions of the brain.
“We are excited about these findings, especially since another anti-tau ASO has already undergone a Phase I clinical trial in people with Alzheimer’s disease,” says Mucke. “It could be useful to consider this strategy also for Dravet syndrome and related conditions. However, defining the optimal timing for treatment initiation will be key, as the window of opportunity might be quite narrow.”
Although Alzheimer’s disease, epilepsy, and autism have diverse causes, they all seem to be associated with abnormally high ratios between excitatory and inhibitory neuronal activities—and this abnormality could potentially be fixed by tau-lowering therapeutics.
Still, a treatment based on anti-tau ASOs would involve repeated spinal taps, a procedure most people would rather avoid. Therefore, Mucke is partnering with Takeda Pharmaceuticals to develop small molecules that could reduce brain tau levels when administered as a pill.
For Media
Julie Langelier
Associate Director, Communications
415.734.5000
Email
About the Study
The paper “Tau ablation in excitatory neurons and postnatal tau knockdown reduce epilepsy, SUDEP, and autism behaviors in a Dravet syndrome model” was published in the journal Science Translational Medicine on April 27, 2022.
Additional authors include co-first author Che-Wei Chang, Xinxing Yu, Kaitlyn Ho, Michelle Zhang, Xin Wang, Jeffrey Simms, Iris Lo, Jessica Speckart, Julia Holtzman, and Gui-Qiu Yu from Gladstone, as well as Zhiyong Li and Erik D. Roberson from UC San Francisco.
This work was funded by the National Institutes of Health (grants R01 MH115679, P01 AG073082, and R01 NS075487), the BrightFocus Foundation, and the Alzheimer’s Association.
About Gladstone Institutes
Gladstone Institutes is an independent, nonprofit life science research organization that uses visionary science and technology to overcome disease. Established in 1979, it is located in the epicenter of biomedical and technological innovation, in the Mission Bay neighborhood of San Francisco. Gladstone has created a research model that disrupts how science is done, funds big ideas, and attracts the brightest minds.
Support Discovery Science
Your gift to Gladstone will allow our researchers to pursue high-quality science, focus on disease, and train the next generation of scientific thought leaders.
Disrupted Boundary Between Cell Types Linked to Common Heart Defects
Disrupted Boundary Between Cell Types Linked to Common Heart Defects
Gladstone scientists identified a cellular boundary that guides heart development and revealed how disrupting it can lead to holes in the heart’s wall.
News Release Research (Publication) Congenital Heart Disease Cardiovascular Disease Bruneau LabGene Editing Strategy Could Treat Hundreds of Inherited Diseases More Effectively
Gene Editing Strategy Could Treat Hundreds of Inherited Diseases More Effectively
Scientists at Gladstone show the new method could treat the majority of patients with Charcot-Marie-Tooth disease.
News Release Research (Publication) Neurological Disease Conklin Lab CRISPR/Gene EditingGenomic Maps Untangle the Complex Roots of Disease
Genomic Maps Untangle the Complex Roots of Disease
Findings of the new study in Nature could streamline scientific discovery and accelerate drug development.
News Release Research (Publication) Marson Lab Genomics Genomic Immunology