Gladstone NOW: The Campaign Join Us on the Journey✕
Gladstone scientists discovered a way to enhance the efficiency of stem cell reprogramming with a gene mutation that causes “stone man syndrome.” [Photo: Chris Goodfellow, Gladstone Institutes]
How do you improve a Nobel Prize-winning discovery? Add a debilitating disease-causing gene mutation.
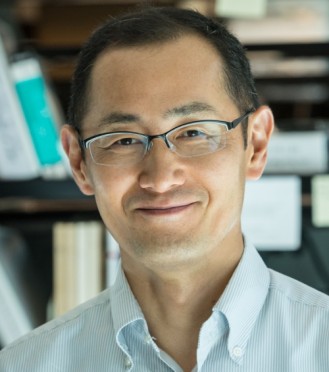
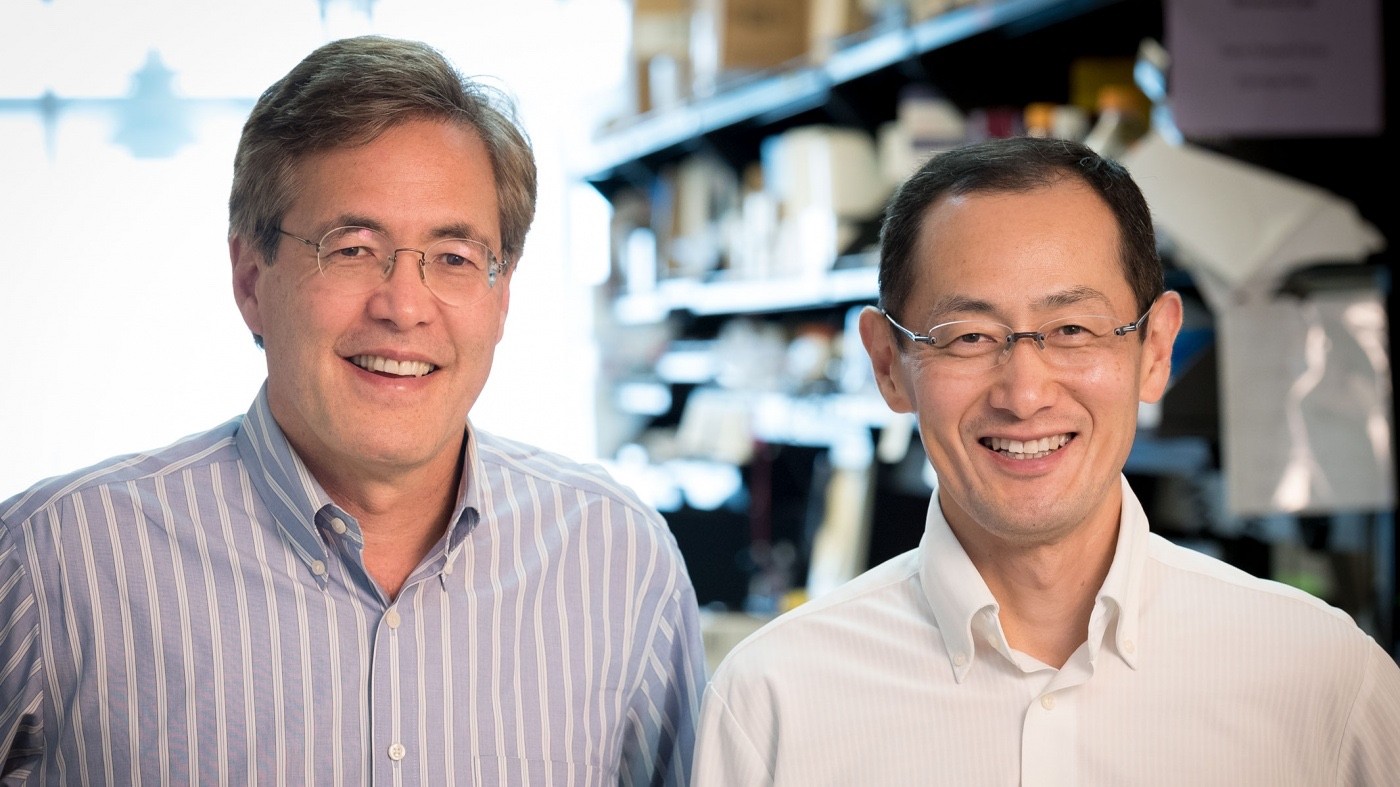
In a study published in the journal Proceedings of the National Academy of Sciences, Shinya Yamanaka, MD, PhD, who first created induced pluripotent stem cells (iPSCs), and his colleagues at the Gladstone Institutes found a way to increase the efficiency of stem cell reprogramming through research on a rare genetic disease.
iPSCs—stem cells created from skin cells that can be transformed into any type of cell in the body—revolutionized biomedical science. They have contributed to breakthroughs in regenerative medicine and drug discovery, surpassing what researchers once thought possible. But like any new technology, there is room for improvement. For example, using existing techniques, fewer than one percent of adult skin cells are reprogrammed into iPSCs.
“Inefficiency in creating iPSCs is a major roadblock toward applying this technology to biomedicine,” said Yamanaka, a senior investigator at Gladstone and director of the Center for iPSC Research and Application (CiRA) in Japan. “Our study identified a surprising way to increase the number of iPSCs that we can generate.”
The scientists started with a very different goal: to create a cellular model to study fibrodysplasia ossificans progressiva (FOP). This extremely rare genetic disease causes muscle, tendons, and ligaments to turn into bone, earning it the nickname “stone man syndrome.” It is caused by a mutation in the ACVR1 gene, which over-activates a cellular signaling process that is important for embryo development and involves a protein called BMP.
Surprisingly, the scientists discovered that they could create more iPSCs from cells taken from FOP patients than those taken from healthy individuals. They believe this is because BMP signaling enhances cell renewal—a cell’s ability to replicate—and keeps them in a pluripotent state, able to turn into any type of cell. These two traits are key characteristics of stem cells. To confirm their hunch, the researchers prevented BMP signaling, which resulted in fewer iPSCs being generated from FOP patients’ cells. Conversely, activating the signaling pathway yielded more iPSCs.
“Originally, we wanted to establish a disease model for FOP that might help us understand how specific gene mutations affect bone formation,” said first author Yohei Hayashi, PhD, a former postdoctoral scholar in Yamanaka's laboratory. “We were surprised to learn that cells from patients with FOP reprogrammed much more efficiently than cells from healthy patients. We think this may be because the same pathway that causes bone cells to proliferate also helps stem cells to regenerate.”
“This is the first reported case showing that a naturally occurring genetic mutation improves the efficiency of iPSC generation,” added co-author Bruce Conklin, MD, a senior investigator at Gladstone. “Creating iPSCs from patient cells carrying genetic mutations is not only useful for disease modeling, but can also offer new insights into the reprogramming process.”
Featured Experts
Want to Join the Team?
Our people are our most important asset. We offer a wide array of career opportunities both in our administrative offices and in our labs.
Explore CareersVitamin B3 Therapy Offers Hope for Fatal Childhood Disease
Vitamin B3 Therapy Offers Hope for Fatal Childhood Disease
A new framework that matches vitamins with genetic diseases helped uncover that high-dose vitamin B3 can dramatically extend survival in mice with NAXD deficiency.
News Release Research (Publication) Rare Diseases Jain LabEditing Scripts
Editing Scripts
College student Delaney Van Riper describes what it’s like to live with a genetic disorder
Profile Rare Diseases Conklin Lab CRISPR/Gene EditingGladstone Rare Disease Research Promises Big Payoff
Gladstone Rare Disease Research Promises Big Payoff
With support from the Wilsey Family, Gladstone is studying a rare genetic condition that could provide clues to curing a whole host of diseases.
Philanthropy Stem Cells/iPSCs Rare Diseases