Gladstone NOW: The Campaign Join Us on the Journey✕
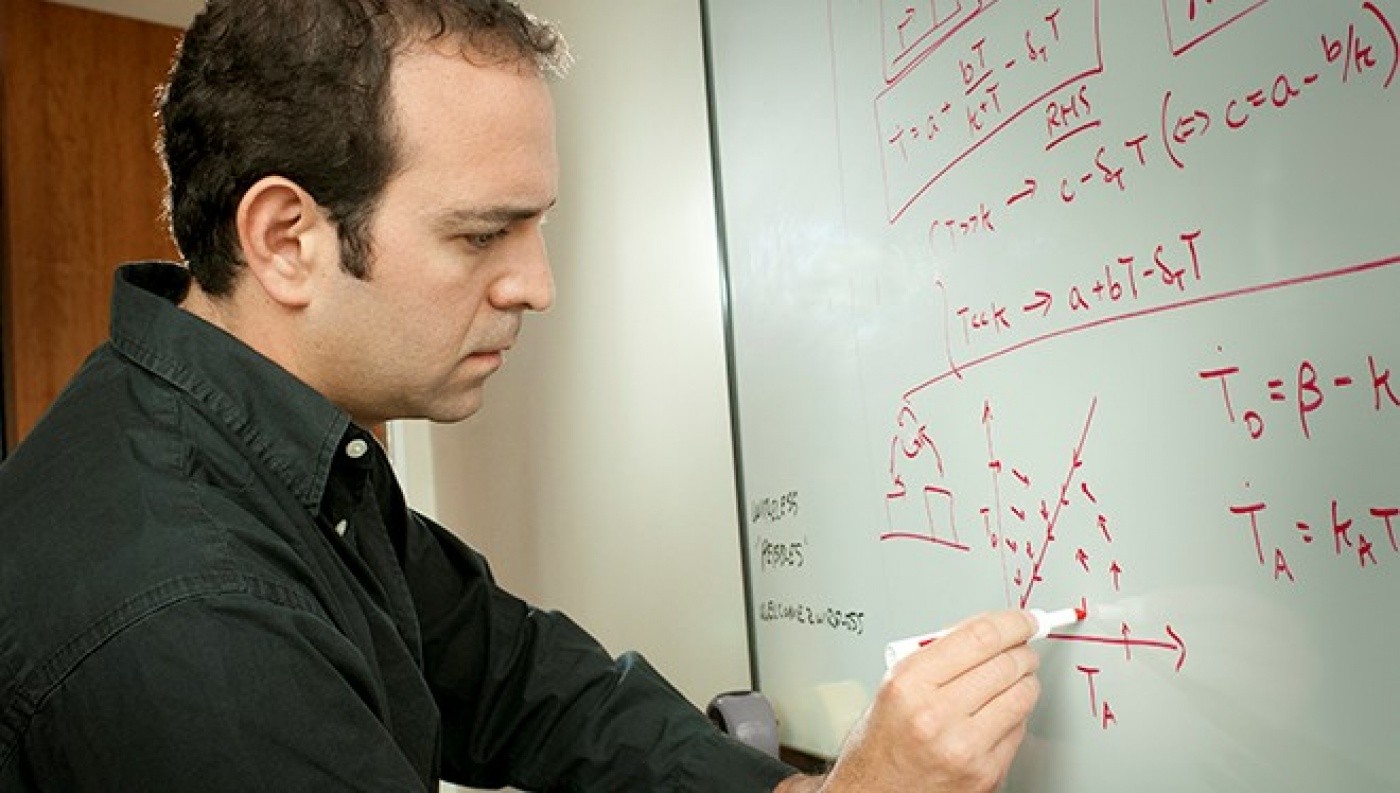
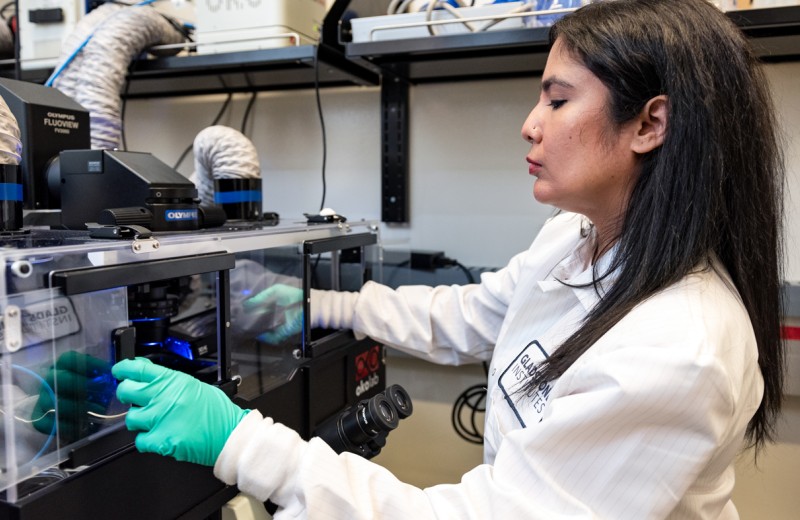
Dr. Weinberger's groundbreaking discovery challenges the conventional theory that infected host cells control latency and could open the door to new pathways. [Photo: Chris Goodfellow]
New research from the Gladstone Institutes for the first time provides strong evidence that HIV latency is controlled not by infected host cells, but by the virus itself. This fundamentally changes how scientists perceive latency, presenting it as an evolutionarily advantageous phenomenon rather than a biological accident.
Viral latency is one of the premier challenges in developing a cure for HIV. Latency causes the virus to go into hibernation, enabling it to escape eradication by currently available antiretroviral therapies. The prevailing view has been that latency is an unintended byproduct of the host cell’s natural life cycle; the infected immune cell naturally “relaxes” into a resting state, incidentally causing the virus to be suppressed.
However, a pair of articles published in the journal Cell turn this model on its head, proposing that the virus itself—not the body’s immune cells—controls when HIV is in the latent or active state. What’s more, the researchers suggest that latency is a naturally selected tactic employed by the virus to increase infection rates.
“Latency has been seen as an accident, a lucky break for HIV that allows the virus to avoid eradication by modern drug therapies,” says Leor Weinberger, PhD, an associate investigator at the Gladstone Institutes and senior author on the two papers. “These new data indicate that latency is far from an accident—it is encoded in the virus’s circuitry and is an evolutionarily advantageous strategy, likely increasing the odds of infection by a substantial amount.”
To demonstrate this, the researchers first showed that the virus remains highly active as infected cells transition to resting, suggesting the two processes are independent. Next, with the help of computer modeling, the scientists identified the protein Tat as the crucial mechanism in the virus that controls its on/off switch. In the models, manipulating Tat levels consistently changed the state of the virus, while altering the host cell’s state had little to no impact on viral latency. Finally, to confirm their findings, the researchers used synthetic biology to create simplified viral circuits and directly manipulated Tat independent of the cell in these synthetic viruses. Once again, changing Tat levels was sufficient to turn the virus on or off, and relaxing or activating the host cell did not affect viral expression.
“It’s very difficult to activate the virus without waking up the cell,” explains Anand Pai, PhD, a postdoctoral fellow at Gladstone who co-led the first study. “Using synthetic biology, we were able to effectively decouple the virus and the cell for the first time. This helped reveal that the virus has the ability to control whether it is active or latent, independent of the host cell.”
In the second paper, a collaboration with Ariel Weinberger, PhD, from the Wyss Institute at Harvard University, the investigators used the financial theory of “bet-hedging” to explain why HIV might have evolved a hardwired latency program.
During initial infection, HIV is at high risk for extinction because mucosal tissue—the typical entry point for the virus—is a particularly volatile environment for HIV, with few target cells available that can be infected. If HIV killed off all of the infected target cells upon transmission, the virus would die out, as there would be nowhere left for it to spread. However, if HIV enters a latent state in some of the cells, it can remain off until that cell is transferred to another type of tissue with more abundant target cells, increasing the virus’s odds for successful infection.
To test if this bet-hedging strategy was evolutionarily advantageous for the virus, the scientists generated mathematical models weighing the benefits and drawbacks of viral latency. In each model, based on real patient data, it was beneficial for HIV to go into a latent state, resulting in significantly higher rates of infection than if it did not. This strongly supports the theory that latency is a sophisticated bet-hedging strategy evolved by the virus over millions of years.
“This discovery changes our perspective on HIV latency and contributes to our understanding of what it is going to take to cure HIV,” says Robert Gallo, MD, director of the Institute of Human Virology at the University of Maryland School of Medicine, who co-discovered HIV as the cause of AIDS. “By revealing how and why latency is established and maintained, we may be able to develop new avenues to treat it—something current antiretroviral therapies do not address.”
New Antiviral Therapy May Block COVID-19 Transmission
New Antiviral Therapy May Block COVID-19 Transmission
The single-dose, intranasal treatment also reduces symptoms of multiple variants of the SARS-CoV-2 virus
News Release Research (Publication) COVID-19 Center for Cell Circuitry Infectious Disease Weinberger Lab ChaturvediThrowing Drug Resistance for a Loop
Throwing Drug Resistance for a Loop
New class of resistance-proof drugs could one day transform treatments for viral diseases
News Release Research (Publication) Center for Cell Circuitry Infectious Disease Weinberger Lab ChaturvediGladstone Science Has Three Chances to Win STAT Madness
Gladstone Science Has Three Chances to Win STAT Madness
Gladstone discoveries compete head-to-head with other scientific advancements
Awards COVID-19 Traumatic Brain Injury Alzheimer’s Disease Huang Lab Paz Lab Weinberger Lab Chaturvedi