Gladstone NOW: The Campaign Join Us on the Journey✕

Gladstone started as a single institute focused on cardiovascular disease. It has since grown to four institutes which use cutting-edge technology to tackle cardiovascular, neurological, and immunological diseases.
The evolution of research at Gladstone Institutes began 40 years ago with seven people in a borrowed conference room with a card table and a telephone at San Francisco General Hospital. This team of scientists, led by a 37-year-old biochemist named Robert Mahley, MD, PhD, had spent the previous 8 years at the National Institutes of Health, probing the world’s number one killer, heart disease, an epidemic that ripped through the developed world, accounting for 40 percent of deaths.
But they’d been recruited to the Bay Area by the Gladstone trustees to establish a new research institute where the best scientists would contribute to the understanding of heart disease, developing preventions and cures, and transforming biomedical research. How to get there was left up to the scientists.
“That’s been our philosophy from the start. It’s part of our culture: hire the best people and encourage them to follow wherever the science leads. In fact, that’s our expectation,” said Mahley, Gladstone’s founding president, who guided the organization for 30 years, before stepping down as the president and returning to his research.
Gladstone began as a single entity with a single purpose. But as the scientists followed the science—unencumbered by the red tape of bureaucracy—the purpose, and the focus, grew.
From Prevention to Regeneration
Mahley brought a diverse team of researchers to Gladstone: an organic chemist, a cell biologist, a protein chemist, a lipid biochemist, a clinician, and a research associate. Their work was entirely focused on heart disease, particularly atherosclerosis, a disease that causes the buildup of lipids and cholesterol in the artery wall that blocks blood flow and can cause a heart attack. That inevitably led them to study plasma lipoproteins, molecules that transport cholesterol in the blood.
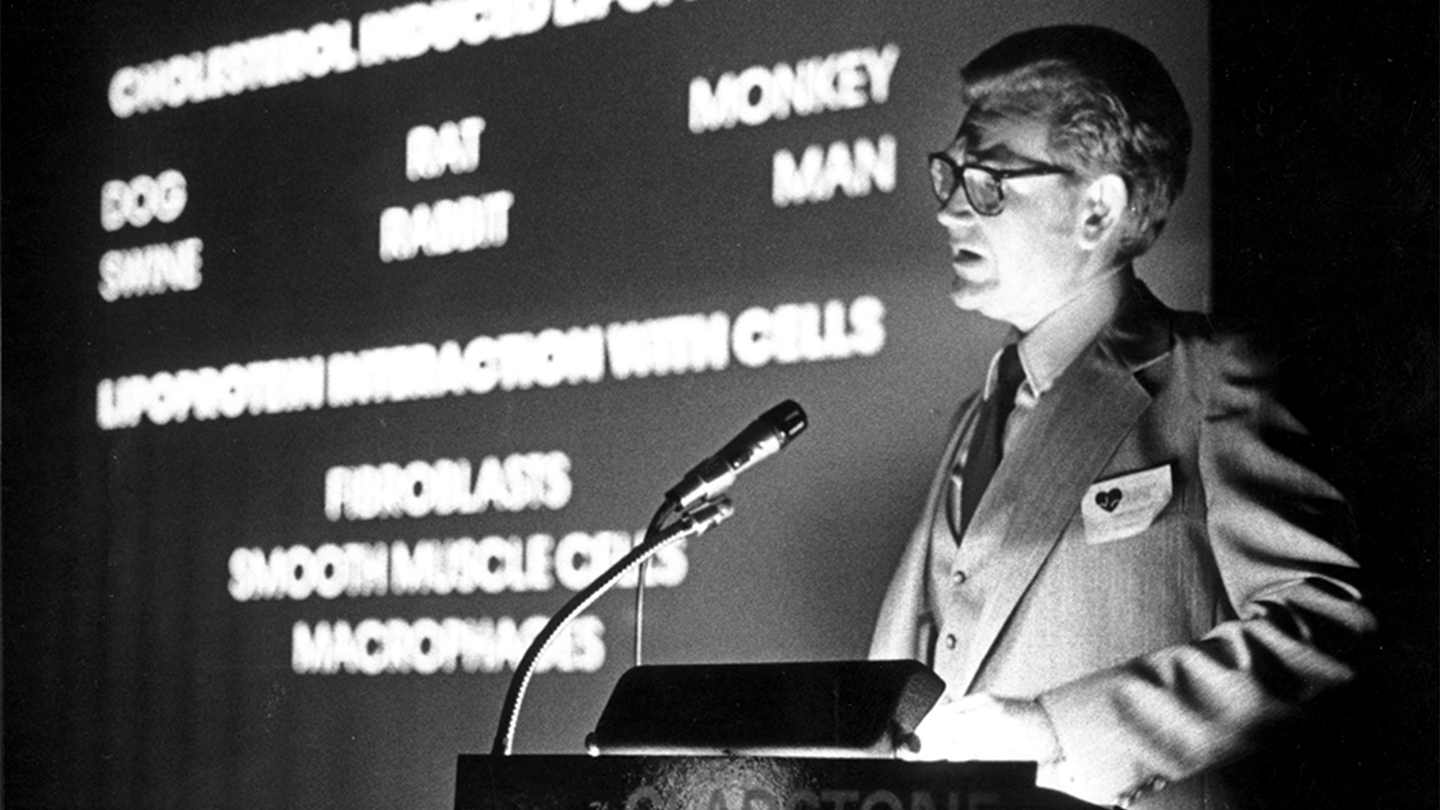
Robert Mahley became the founding president of the Gladstone Foundation Laboratories in 1979.
“Our mission was to understand in detail those proteins, specifically one called apoB and also a protein called apoE,” Mahley explained. “Our scientists were able to understand the mechanism whereby cholesterol was delivered to cells. This work contributed, in part, to the development of the statins, which are for many of us, miracle drugs. Prior to the development of the statins, we had very limited ways in which to lower blood cholesterol, which is the major risk factor for heart disease.”
The rate of deaths related to heart disease has decreased from 40 percent to 25 percent since the introduction of statins.
“Though it is still the leading cause of death in the United States and in most of the world, it certainly does not have the same impact that it had before we really understood lipoprotein metabolism and before we had the drugs that would reduce cholesterol levels,” said Mahley.
Adding the ‘s’
By 1990, with about a dozen scientists now on board and a budget of $9 million, “the trustees had reached a point where they had to make a decision,” said Mahley. “Should they just continue growing the cardiovascular research area or apply this unique model of bringing in teams of investigators to tackle a new emerging health problem?”
Added Mahley, “We wondered, ‘should we diversify?’” It was a rhetorical question in Mahley’s mind. He wanted to expand Gladstone’s focus, and impact, and the trustees agreed with him. Around that time, San Francisco was the epicenter for a rapidly growing international epidemic of HIV/AIDS, with no cure in sight. Mahley was serving on a search committee at UC San Francisco (UCSF), that was looking for a director to lead the new HIV/AIDS research center being planned.
They soon identified the person they wanted to be the director—Warner Greene, MD, PhD, a molecular biologist who was leading HIV research at Duke University. Unfortunately, UCSF lacked the necessary resources to complete the project, so Gladstone took the proverbial ball and ran with it in coordination with UCSF, moving into HIV/AIDS research. Greene moved to San Francisco in 1991.
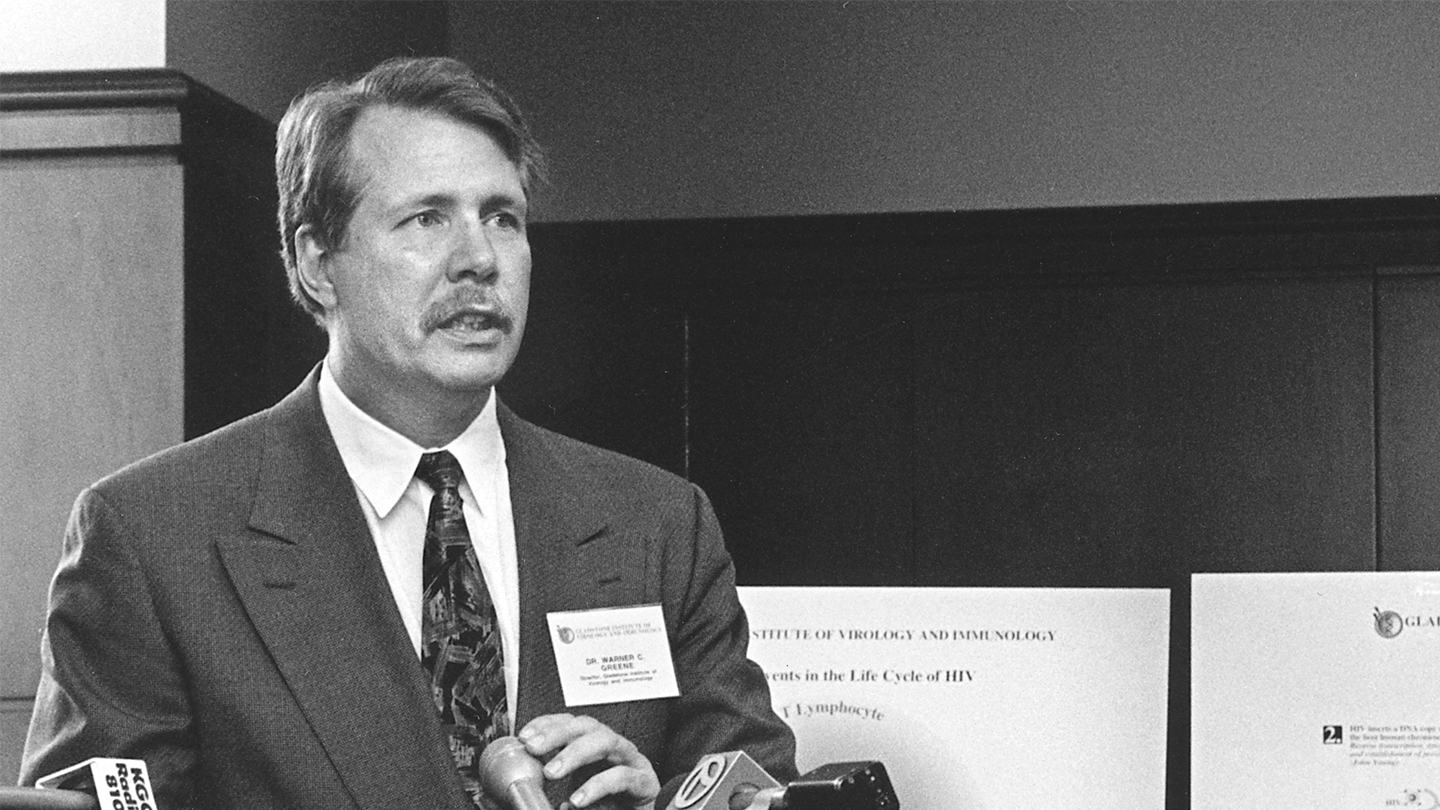
The Gladstone Institute of Virology and Immunology was launched in 1992, with Warner Greene as its founding director.
Gladstone officially became ‘institutes’ in 1992, with the beginning of the Gladstone Institute of Virology and Immunology, which was also located at San Francisco General Hospital.
“That put us very close to the clinicians and the patients. And that was wonderful in terms of being able to start doing patient-based research,” said Greene, who was employee number one at the institute, and had to build a team of investigators. “And I was also trying to create a vibrant relationship with fellow scientists at UCSF.”
Unfortunately, while the hospital was a great place to study HIV, Greene’s colleagues were mostly located across town at UCSF’s Parnassus campus. And the work itself, of course, could be profoundly challenging. Those first couple of years, Greene attended the medical wards at the hospital.
“Every patient that was admitted to my service was infected with HIV. Every single patient,” said Greene. “And there was hardly a thing we could do. We would chase one opportunistic infection after another. We had no antiretroviral therapy at this point. All of the patients died.”
But Greene and his team were learning more about the virus, which led to the advent of rational drug screening. By the mid-1990s, Greene said, “we had combination antiretroviral therapy, multiple drugs. It takes multiple drugs because of the highly mutagenic nature of the virus, which was always changing. The drugs were an absolute miracle, transforming HIV/AIDS from an acute death sentence to a chronic, manageable disease. Not like cancer, but more like diabetes. So these drugs were just remarkable. They will go down in the history of medicine as one of the great accomplishments.”
Greene’s team of researchers helped solve some of the mysteries behind the disease. They showed that a major cause of CD4 T-cell depletion was damage to the thymus, then demonstrated that human growth hormone could re-energize the thymus and restore or increase CD4 T-cell production. They conducted the first pivotal trial, across 19 countries, proving that antiretroviral drugs could prevent high-risk individuals from becoming infected. This is now the standard for prophylaxis worldwide. They showed how CD4 T cells die during HIV infection. Surprisingly, these cells were not lost because of a toxic effect of the virus but rather because of the host response against the virus—a suicide, not a murder.
While it’s difficult to draw a straight line defining the precise evolution from basic scientific research into these world-changing therapeutics, Greene said, “everything that we learned and understood about the virus, like the function of its nine different genes and its life cycle, led to new therapeutic opportunities. Today I would say it’s possible, with over 30 drugs, to suppress to undetectable levels the viremia in all individuals. Now, about 23 million of the more than 38 million people with HIV are receiving antiretroviral therapy. That is spectacular.”
But the work isn’t done yet, not by a long shot.
“We don’t have a cure, we don’t have a vaccine, and the epidemic is not shrinking,” Greene said. “We are at a tipping point. Will the developed world continue to invest the billions and billions of dollars needed every year for antiretroviral therapy in Africa? If we could come up with a treatment and cure individuals with one shot and you’re done, well that would be a game changer for the world.”
Meanwhile, Gladstone virologists are following their science into other realms of human health. “Gladstone has broadened its area of research beyond HIV to other viruses that are still wreaking havoc worldwide,” said Deepak Srivastava, MD, who became president of Gladstone in January 2018. “In the process of doing that, we’ve learned a lot about the interplay between viruses and other pathogens and the immune system. That has taught us not just about viruses but also about how the immune system responds.” It’s becoming increasingly clear that the immune system could be harnessed to tackle a number of human diseases and this will be a growing focus of Gladstone in the coming years.
Heady Days
Throughout its history, Gladstone’s research evolution has been directed by the scientists’ response to major biomedical and societal challenges in the world. The creation of the Gladstone Institute of Neurological Disease was a response to the realization that neurodegenerative diseases (e.g., Alzheimer’s, Parkinson’s) were affecting a large and increasing aging population, and could very well overrun the global health care system.
This was also a research institute that Mahley had in mind for years, a direct link to the work that he and fellow researchers in cardiology had been doing. In the mid 1980s, when Mahley and his colleagues were trying to determine where apoE was being made in the body, “We knew that the major site of synthesis of apoE was in the liver, but we found that the second most common site for the production of apoE was in the brain. What was our heart disease protein doing in the brain?”
The institutes emerged from the discovery that a form of apoE called apoE4, was not only “a risk factor for heart disease, but was also the major genetic risk factor for Alzheimer’s disease,” said Mahley. Twenty-five percent of the population has one copy of apoE4, representing just one amino acid change from the “normal” apoE, and this conferred a 3-fold increased risk for Alzheimer’s. People with two copies of apoE4 have a 12-fold increased risk. Because of apoE4’s role in heart disease, Gladstone was the world’s leading knowledge center for this protein, so the new focus had a natural beginning. Mahley had recruited a neurological disease expert named Lennart Mucke, MD, from The Scripps Research Institute to the Bay Area in 1996, and in 1998 they created the third Gladstone institute, with Mucke as its new director.
The Gladstone Institute of Neurological Disease, with roots in Alzheimer’s disease research, “has since been expanded to include related conditions that might overlap with Alzheimer’s disease or have links to it,” explained Mucke, who is still the institute director and a senior investigator.

Lennart Mucke has been the director of the Gladstone Institute of Neurological Disease since its founding in 1998.
“We realized early on that Alzheimer’s disease had multiple causes and wasn't going to be dealt with readily with one blockbuster drug or a single approach, and I think that distinguishes our research program from many others around the country and the world,” Mucke said. “From the get-go, we started a program that really tried to respond to the multiple factors of Alzheimer’s disease, with a multi-pronged plan of attack.” So Mucke put together an interdisciplinary team, figuring they might learn from other conditions that also were dependent on aging and also led to the demise of brain cells. “We recruited people with expertise in Huntington’s disease, Parkinson’s disease, inflammation, energy metabolism, and brain network dysfunction to develop a deep and comprehensive understanding of how major diseases of the nervous system erode the functions that allow us to enjoy and control our lives, share thoughts with loved ones, and improve the world.
“Over the years, our investigators made many groundbreaking discoveries about the processes by which these diseases impair brain functions,” said Mucke. “In addition, we identified promising entry points for therapeutic interventions and developed novel approaches to accelerate the translation of scientific discoveries into better treatments in this challenging area of biomedicine.”
At this stage, 20-plus years into the research program, Gladstone scientists are exploring not only a broad range of neurodegenerative and neuroinflammatory disorders, but also disabling psychiatric conditions, such as autism spectrum disorders, obsessive compulsive disorders, and schizophrenia.
“For each of the neurodegenerative diseases that we study, ranging from Alzheimer's to Parkinson’s, Huntington’s, ALS, and even multiple sclerosis, there are several known different genetic causes, but we believe many of them are interacting with one another and there’s a disruption of the whole network of molecular and neuronal connections,” Srivastava explained.
As Steve Finkbeiner, director of the Gladstone Center for Systems and Therapeutics and a neurologist points out, “It’s becoming clearer that the same gene, when mutated, can cause different diseases. While we have clinically given different diseases distinct names, the problem in each of those settings may be exactly the same, and the beauty of that recognition is that if we find a breakthrough drug for any one disease, it may apply to multiple diseases. That gives me great hope that we’ll actually be able to solve many of these problems in the coming years.”
Change of Heart
In 2005, Mahley recruited Srivastava to direct the Gladstone Institute of Cardiovascular Disease. By then, Mahley had already decided that the institute should move in a new direction. They’d already attacked the cholesterol problem. But there was still the problem of what to do about a damaged heart.
“When a heart attack occurs, the cardiomyocytes, the heart muscle cells, die—they never regenerate, and what replaces them is non-functional scar tissue,” Mahley said.
Srivastava, recruited from the University of Texas, was interested in how heart cells were formed and how they worked together to make an organ. It turned out he was the ideal fit for what lay ahead at Gladstone.
“At the time I arrived here, the field of regenerative medicine and stem cell biology was emerging, and my laboratory’s work for many years had been focused on understanding how nature normally makes a heart, with the idea that we would develop an understanding of why children are born with heart malformations and that we could use that knowledge to regenerate damaged hearts in adults,” Srivastava said.
Information Age
Srivastava wasn’t at Gladstone very long before realizing that basic scientific research was being increasingly driven by technology, and was more data-intensive. “The real challenge is analyzing those data in innovative ways, and asking creative questions to gain new insights,” Srivastava said.
He needed someone with background in this area. He needed someone like Katherine Pollard, PhD, whose training had been in statistics, but who wanted to make a difference in biomedical research.
She joined Gladstone in 2008, at a time when Srivastava was making a concerted effort toward increasing the institutes’ computational biology capacity. “He also made a number of other key recruitments around that time of people who worked in different technology areas, including stem cells, for example, and more recently, in genome editing,” said Pollard. She was excited about establishing a computational lab that would be surrounded by wet labs and liked the idea of using her group’s modeling techniques and bioinformatics tools in an intimate, collaborative setting.

Gladstone launched its fourth institute in 2018 with Katherine Pollard as the founding director.
So Pollard’s team joined the cardiovascular institute and immediately started growing, collaborating with investigators in the other institutes, “getting grants with them, writing papers with people in all three disease areas,” she said. “I think it was a natural transition to not be housed within a single disease area but to recognize that my lab and some of the other technology-driven labs at Gladstone are here because we want to make an impact across multiple disease areas, and we are developing research platforms that are designed to be useful across disease areas.”
Her role evolved from being a principal investigator inside the institute of cardiovascular disease into becoming director of Gladstone’s fourth institute, the Gladstone Institute of Data Science and Biotechnology.
Pollard has identified the three most important components in realizing a vision for the new institute: “We need the biomedical contexts for the diseases that we’re working on. We need the experimental technologies. And then also, we need the data scientists all talking together and working as a team. I believe that if you put the data scientists more upstream in the process and in a more peer-to-peer role and a more interactive and iterative role, we can build better research technologies by thinking ahead about how we want to use the data and how to build machines so that we get the data and the knowledge out of them that we need to. And very importantly, doing that here at Gladstone, it’s not just technology development for the fun of it, but really geared toward trying to answer biomedical questions.”
The lines between labs are almost non-existent now as the tendrils of collaboration stretch out in all directions at Gladstone, where researchers now use artificial intelligence and machine learning to analyze massive sets of data across all disease areas.
“We believe it’s the tight intertwining of data science and cutting-edge technologies with disease biology that is really going to create the magic here,” said Srivastava, offering a few examples of Gladstone’s investment in that kind of magic, such as in the stem cell field, where the Roddenberry Stem Cell Center at Gladstone provided resources and infrastructure for new stem cell approaches across all the disease areas.
“Similarly, we’ve made a major investment in CRISPR-based gene-editing technologies and use of CRISPR for a variety of other genomic types of experiments,” he said. “All the disease areas are being affected by this new technology, which allows us to do the types of experiments that we could never do before.”
The Path Ahead
Gladstone has some powerhouse researchers under its roof—for example, the founder of induced pluripotent stem cell technology (2012 Nobel Prize winner Shinya Yamanaka) and the co-inventor of CRISPR gene-editing technology (Jennifer Doudna), which helps when considering what may lie ahead. The technologies they’ve developed will have ramifications in every disease area Gladstone scientists are delving into, including the problems on which Gladstone was founded.
In addition, artificial intelligence and computational methods, in particular, have the potential to truly transform science. As Gladstone researchers team up with computer scientists to develop powerful algorithms and machine learning tools, they are increasing their capacity to identify patterns in huge datasets of biological information and reveal unknown connections to human disease. This will significantly accelerate the rate of scientific discovery and the development of novel therapies.
“I consider this the golden era of science,” Srivastava said. “That’s because we’ve spent the last several decades building a foundation of knowledge about how human cells work and we’ve built a number of tools and technologies that allow us to deeply interrogate human cells from any patient with any disease.
“We can sequence human genomes at a scale where hundreds of thousands of people are having their genome sequenced. It will soon be millions and will eventually be everybody, and that allows us an opportunity to connect genetic changes with susceptibility to disease and with that, understanding. I don’t see clear obstacles preventing us from finally creating directed therapeutics for many of the diseases that right now are completely unsolved.”
Support Discovery Science
Your gift to Gladstone will allow our researchers to pursue high-quality science, focus on disease, and train the next generation of scientific thought leaders.
From Mentorship to Legacy: Creating Opportunity for Early Career Scientists
From Mentorship to Legacy: Creating Opportunity for Early Career Scientists
Robert and Linda Mahley’s commitment to trainee development continues through Gladstone’s annual Career Advancement Awards.
Graduate Students and Postdocs HistoryGladstone Mourns the Loss of Founding Trustee Richard D. Jones
Gladstone Mourns the Loss of Founding Trustee Richard D. Jones
Jones lent Gladstone his time and expertise for nearly 50 years.
History Institutional NewsRemembering Bill Rutter, a Biotech Visionary and Champion of Gladstone
Remembering Bill Rutter, a Biotech Visionary and Champion of Gladstone
William J. Rutter, PhD, was a pioneering force in biomedicine whose vision shaped San Francisco’s Mission Bay neighborhood into a hub for innovation and discovery.
History Profile



