Gladstone NOW: The Campaign Join Us on the Journey✕

SAN FRANCISCO, CA—Scientists at the Gladstone Institutes have mapped the molecular mechanism by which a virus known as cytomegalovirus (CMV) so successfully infects its hosts. This discovery paves the way for new research avenues aimed at fighting this and other seemingly benign viruses that can turn deadly.
Not all viruses are created equal. Some ravage the body quickly, while others—after an initial infection—lie dormant for decades. CMV is one of the eight types of human herpes viruses, a family of viruses that also include Epstein-Barr virus (which causes mononucleosis) and varicella-zoster virus (which causes chickenpox), and it is one of the world’s most rampant. And like other successful viruses, CMV maintains a few key features: it replicates quickly, it evades the host’s immune defenses and it keeps the host cell alive just long enough to produce optimal amounts of virus. This last feature helps prevent the virus from building up to toxic levels inside a cell—an action that would kill the cell before the virus had a chance to spread to neighboring cells. To achieve this delicate balance, CMV applies a ‘braking mechanism’ after initial replication inside the cell. But the underlying process behind this mechanism has long eluded scientists.
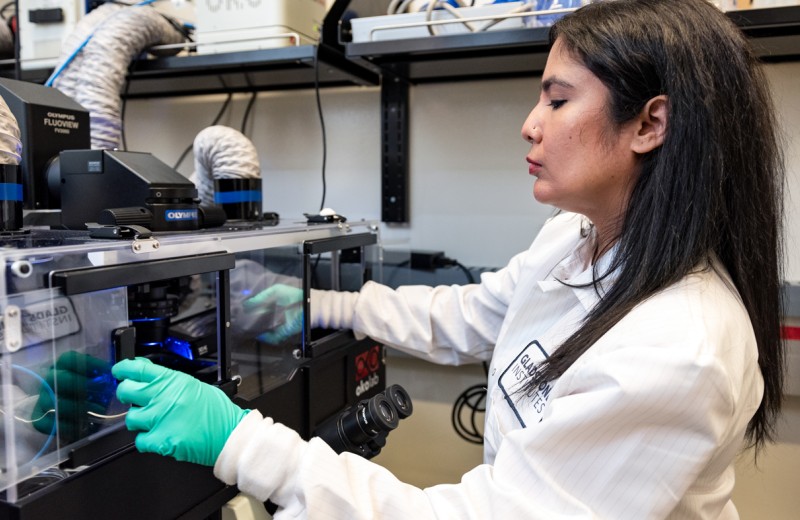
Today, researchers in the laboratory of Gladstone Investigator Leor Weinberger, PhD, announce the key to CMV’s success: a type of ‘accelerator circuit’ hidden within the virus’ DNA that lets CMV reach optimal levels quickly before the host cell has time to respond—but that also stops the virus from killing the cell before those optimal levels are reached. They report their findings in the latest issue of the journal Cell, now available online.
“CMV infects between 50% and 80% of adults worldwide and can often be transmitted from mother to child during pregnancy,” said Dr. Weinberger, who is also an associate professor of biochemistry and biophysics at the University of California, San Francisco (UCSF), with which Gladstone is affiliated. “While CMV usually lies dormant, it can be dangerous or even deadly for the developing fetus or for those with compromised immune systems—such as organ-transplant recipients. As a result, we have long sought to understand exactly how CMV infects cells, in the hopes of developing treatments or a vaccine to diminish its presence around the world.”
Dr. Weinberger and his team focused on a small stretch of DNA in CMV’s genetic code. Known as Major Immediate-Early Promoter (MIEP), this genetic code kick-starts viral replication by generating IE2, a protein that can be extremely toxic in large quantities. And within MIEP the team discovered the real instigator of viral replication.
In a series of experiments, the team found that when MIEP is activated it not only generates IE2 and spurs replication, but it also cues the virus to stop generating the toxic IE2 protein at the precise moment when optimal levels of IE2 have been reached.
“CMV needs IE2 in order to replicate inside the host cell, but if too much IE2 is produced too quickly, the host cell will be killed before CMV has a chance to spread,” said Melissa Teng, a graduate student at the University of California, San Diego (UCSD), a visiting UCSF graduate student and one of the paper’s lead authors “But CMV gets around this problem with the so-called ‘accelerator circuit,’ which helps maintain optimal IE2 levels. This circuit allows CMV to replicate quickly and efficiently, infecting a range of cell types throughout the body.”
To confirm these findings, the team infected human cells in dish with two forms of CMV—one of which could generate the IE2 accelerator circuit and one that could not. When they placed both viruses in the same dish, they saw a clear difference. Over time, the viruses without the accelerator circuit disappeared, while the accelerator virus quickly took over the dish. The evidence was clear—this circuit was key to the virus’ success.
“This impressive work demonstrates a new mechanism for how a relatively simple genetic network can respond to external cues and create the most optimal environment for viral replication,” said Gurol Suel, PhD, an associate professor of molecular biology at UCSD who was not involved in the study. “It’s quite likely that mechanisms like this one exist in other biological systems, including other viruses.”
“The accelerator circuit gives CMV the powerful strategic advantage to outpace immune defense systems,” said Gladstone Staff Scientist Cynthia Bolovan-Fritts, PhD, the paper’s other lead author. “The next step is to understand this mechanism on a deeper level and develop therapeutic approaches to target and disrupt the circuit—and hopefully stop viruses such as CMV in their tracks.”
Gladstone Postdoctoral Fellow Roy Dar, PhD, also contributed to this research, which was supported by the National Institutes of Health, the Pew Charitable Trust, the Center for Nanophase Materials Sciences (United States Department of Energy), the National Science Foundation Graduate Research Fellowship Program and the National Cancer Institutes.
New Antiviral Therapy May Block COVID-19 Transmission
New Antiviral Therapy May Block COVID-19 Transmission
The single-dose, intranasal treatment also reduces symptoms of multiple variants of the SARS-CoV-2 virus
News Release Research (Publication) COVID-19 Center for Cell Circuitry Infectious Disease Weinberger Lab ChaturvediThrowing Drug Resistance for a Loop
Throwing Drug Resistance for a Loop
New class of resistance-proof drugs could one day transform treatments for viral diseases
News Release Research (Publication) Center for Cell Circuitry Infectious Disease Weinberger Lab ChaturvediGladstone Science Has Three Chances to Win STAT Madness
Gladstone Science Has Three Chances to Win STAT Madness
Gladstone discoveries compete head-to-head with other scientific advancements
Awards COVID-19 Traumatic Brain Injury Alzheimer’s Disease Huang Lab Paz Lab Weinberger Lab Chaturvedi