Gladstone NOW: The Campaign Join Us on the Journey✕
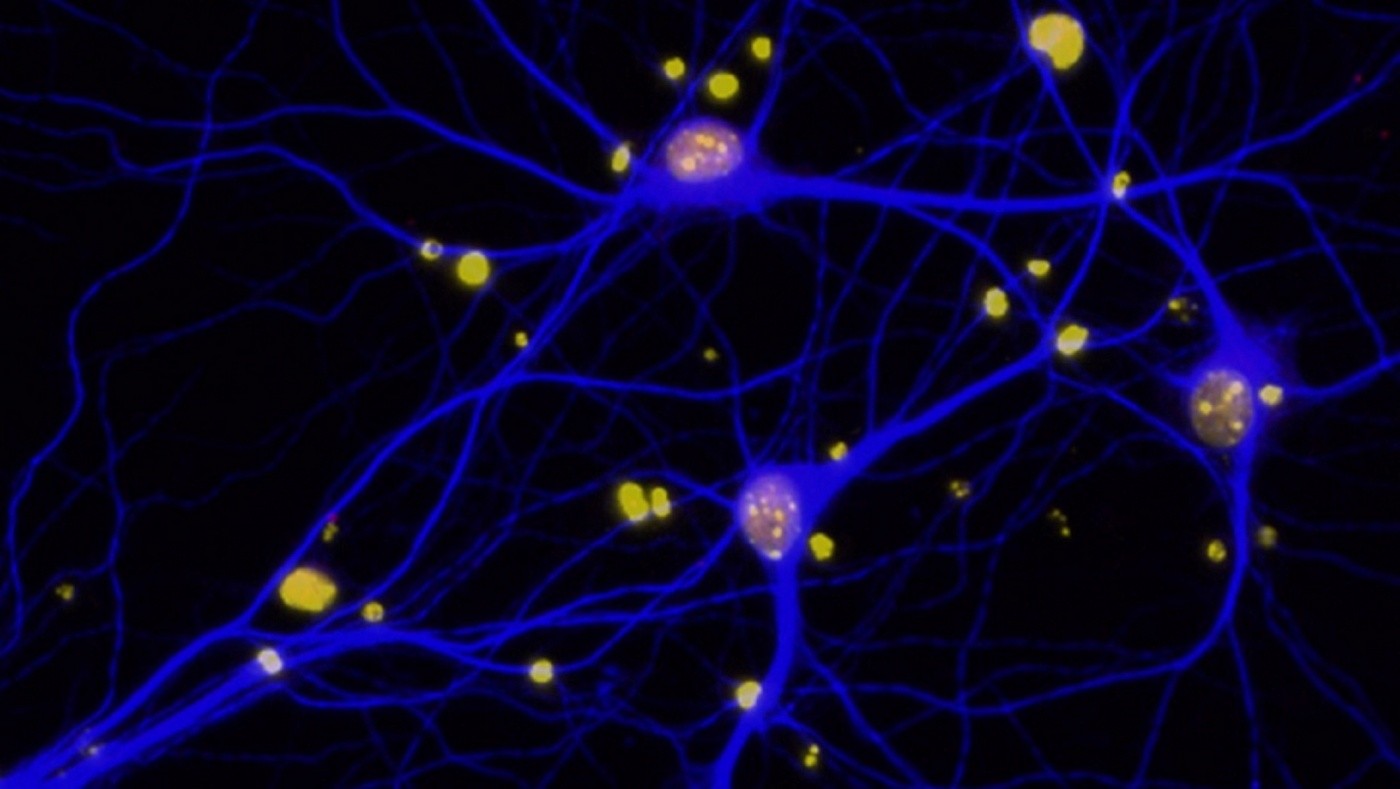
Reduced levels of BRCA1 (red) in neurons (blue). Amyloid-beta plaques in the brain can deplete neurons of BRCA1, contributing to cognitive deficits in Alzheimer's disease. [Image: Elsa Suberbielle]
Researchers from the Gladstone Institutes have shown for the first time that the protein BRCA1 is required for normal learning and memory and is depleted by Alzheimer’s disease.
BRCA1 is a key protein involved in DNA repair, and mutations that impair its function increase the risk for breast and ovarian cancer. The new study, published in Nature Communications, demonstrates that Alzheimer’s disease is associated with a depletion of BRCA1 in neurons and that BRCA1 depletion can cause cognitive deficits.
“BRCA1 has so far been studied primarily in dividing (multiplying) cells and in cancer, which is characterized by abnormal increases in cell numbers,” says first author Elsa Suberbielle, PhD, a research scientist at the Gladstone Institutes. “We were therefore surprised to find that it also plays important roles in neurons, which don’t divide, and in a neurodegenerative disorder that is characterized by a loss of these brain cells.”
In dividing cells, BRCA1 helps repair a type of DNA damage known as double-strand breaks that can occur when cells are injured. In neurons, though, such breaks can occur even under normal circumstances, for example, after increased brain activity, as shown by the team of Gladstone scientists in an earlier study. The researchers speculated that in brain cells, cycles of DNA damage and repair facilitate learning and memory, whereas an imbalance between damage and repair disrupts these functions.
To test this idea, the scientists experimentally reduced BRCA1 levels in the neurons of mice. Reduction of the DNA repair factor led to an accumulation of DNA damage and to neuronal shrinkage. It also caused learning and memory deficits. Because Alzheimer’s disease is associated with similar neuronal and cognitive problems, the scientists wondered whether the problems might be mediated by depletion of BRCA1. They therefore analyzed neuronal BRCA1 levels in post-mortem brains of Alzheimer’s patients.
Compared with non-demented controls, neuronal BRCA1 levels in the patients were reduced by 65-75%. To determine the causes of this depletion, the investigators treated neurons grown in cell culture with amyloid-beta proteins, which accumulate in Alzheimer brains. These proteins depleted BRCA1 in the cultured neurons, suggesting that they may be an important cause of the faulty DNA repair seen in Alzheimer brains. Further supporting this conclusion, the researchers demonstrated that accumulation of amyloid-beta in the brains of mice also reduced neuronal BRCA1 levels. They are now testing whether increasing BRCA1 levels in these mouse models can prevent or reverse neurodegeneration and memory problems.
“Therapeutic manipulation of repair factors such as BRCA1 may ultimately be used to prevent neuronal damage and cognitive decline in patients with Alzheimer’s disease or in people at risk for the disease,” says senior author Lennart Mucke, MD, director of the Gladstone Institute of Neurological Disease. “By normalizing the levels or function of BRCA1, it may be possible to protect neurons from excessive DNA damage and prevent the many detrimental processes it can set in motion.”
Fueling Discovery at the Frontiers of Neuroscience: The NOMIS-Gladstone Fellowship Program
Fueling Discovery at the Frontiers of Neuroscience: The NOMIS-Gladstone Fellowship Program
The NOMIS-Gladstone Fellowship Program empowers early-career scientists to push the boundaries of neuroscience and unlock the brain’s deepest mysteries.
Institutional News Neurological Disease Mucke Lab NOMISInside the Brain: Tackling Neurological Disease at Its Roots
Inside the Brain: Tackling Neurological Disease at Its Roots
For World Brain Day, discover some of Gladstone’s latest breakthroughs in neurological research.
Gladstone Experts Research (Publication) Alzheimer’s Disease COVID-19 Parkinson’s Disease Neurological Disease Akassoglou Lab Corces Lab Huang Lab Mucke LabHope for Alzheimer’s: A Conversation with Gladstone’s Lennart Mucke
Hope for Alzheimer’s: A Conversation with Gladstone’s Lennart Mucke
Mucke, director of the Gladstone Institute of Neurological Disease, discusses what's next for Alzheimer’s research, the role of nonprofit research in developing new therapies, and why he's more hopeful than ever for a future where neurodegenerative diseases are fully treatable—and even preventable.
Alzheimer’s Disease Neurological Disease Mucke Lab Aging