Gladstone NOW: The Campaign Join Us on the Journey✕
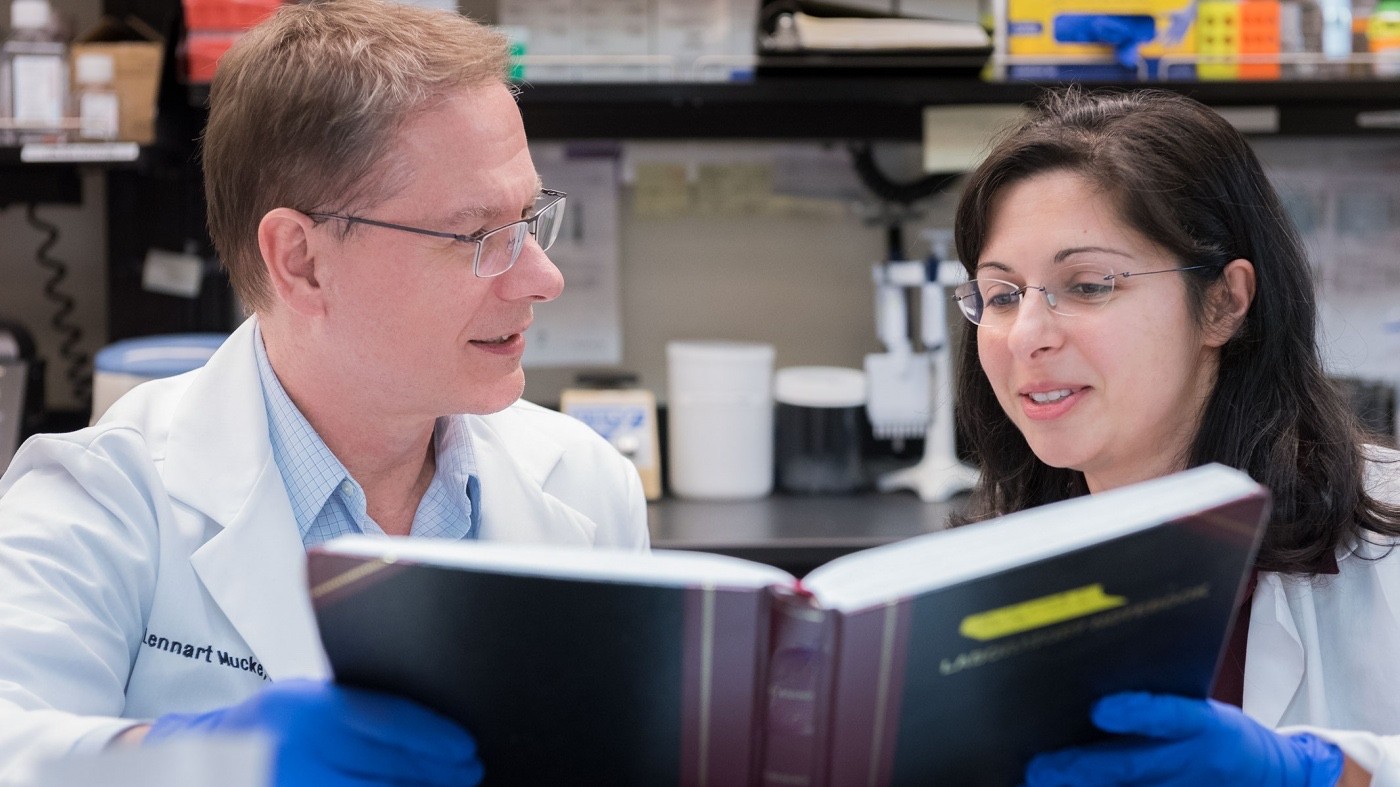
Lennart Mucke, MD, and Jeanne Paz, PhD, have discovered how to control the cacophony of electrical activity in the brain, stopping seizures and reducing deficits related to Alzheimer’s disease. [Photo: Chris Goodfellow, Gladstone Institutes]
Electrical activity in the brain is like a carefully orchestrated symphony, each cell coordinated with its neighbors to fire precisely at the correct time and speed. A seizure is what happens when every instrument starts playing as loud and as fast as it can in the middle of the performance.
Scientists at the Gladstone Institutes are pursuing novel therapies to stop this cacophony in the brain with the goal of treating epilepsy, as well as seizure activity resulting from traumatic brain injury, stroke, or Alzheimer’s disease. They have developed innovative approaches to subdue over-active brain cells and reduce inflammation in the brain to stop seizures and protect against cognitive impairment.
Electricity in the Brain
Epilepsy affects an estimated 3 million Americans, and prolonged seizures and seizure-related accidents kill 50,000 people in the US every year. This condition can be inherited or caused by head injuries, strokes, brain tumors, or neurodegenerative diseases such as Alzheimer’s.
All types of epilepsy are the result of abnormal brain activity, regardless of how it starts or whether it manifests as a typical convulsive seizure or as a more subtle seizure that causes a person to be confused, feel odd, or momentarily lose awareness of what they are doing or what is happening to them.
Millions of electrical signals travel throughout the brain, carrying information from cell to cell and region to region. The cells fire at different speeds and in different patterns, depending on the action being performed. For example, a brain at rest fires in a very different pattern than a brain concentrating on a math problem.
During a seizure, the normal patterns of electrical activity are disrupted, and the cells start to fire at the same pace all at once. This hyper-synchronization results in a surge of electrical activity that causes the brain to malfunction, like a computer with a short circuit.
Controlling the Conductor
Epilepsy researcher Jeanne Paz, PhD, an assistant investigator at Gladstone, found a way to stop seizures as soon as they start by targeting an area of the brain called the thalamus.
“The thalamus is like the conductor in the brain,” explained Paz. “It can generate and control rhythms, and it keeps the brain in tempo. This makes it an ideal target for controlling epilepsy, regardless of where the seizures start.”
The thalamus receives signals from various areas of the brain and shoots them off to other regions. It is particularly well connected to the cortex, the top layer of the brain that controls key abilities like speech, movement, and cognition. The thalamus and cortex create a feedback loop that is heavily implicated in seizures. When cells in one area fire abnormally, it creates a domino effect, triggering seizure activity in the other region, which quickly spreads all over the brain.
In an ingenious move, Paz used this loop to her advantage—she discovered that by blocking activity in the thalamus in animal models of epilepsy, she was able to stop seizures in their tracks. To achieve this, Paz employed a technique called optogenetics, by which specifically tagged brain cells can be regulated with lasers or chemicals. Her team developed a program that monitors the brain for seizures in real-time. When a seizure is detected, the system activates a laser that targets cells in the thalamus and shuts them off. Using this technique, she could immediately interrupt a seizure, regardless of where it started.
“We showed for the first time that manipulating only one type of cell is sufficient to control seizures. Ramping up the firing of cells in the thalamus can initiate a seizure, and turning off those cells can stop it,” Paz said.
Paz first demonstrated this effect in focal seizures that were triggered by a stroke in the cortex and indirectly altered the thalamus. In later experiments, she investigated whether the treatment was also effective in models of generalized childhood epilepsy caused by genetic mutations. In many patients, this type of epilepsy is resistant to current drug therapies. If left untreated, it can be devastating to a child’s life because of the frequent occurrence of seizures, in some cases recurring hundreds of times a day.
“Generalized seizures are like an explosion in the brain. No matter where they start, within milliseconds they spread to many different structures. This lack of focus makes them much harder to target.” Paz explained. “Remarkably, even though the thalamus is not obviously damaged in this type of epilepsy, we were still able to stop seizures in the entire brain by targeting just this one structure.”
Designing a Better Drug
Paz also thinks that chronic inflammation in the thalamus may be behind the dramatic rise in epilepsy following brain damage. Inflammation in the brain is involved in many neurological conditions, including epilepsy, and it is particularly common after brain damage from a stroke or traumatic brain injury. Many brain-damaged patients develop epilepsy, often with debilitating consequences, including sudden death.
“After an injury to the cortex, chronic inflammation can emerge, not only at the site of the lesion, but also in the thalamus. Such inflammation also occurs in patients with intractable epilepsy—those that are least likely to respond to treatment. We want to know if we can prevent epilepsy by avoiding or reversing the chronic inflammation.”
There is typically a latent period after a stroke or injury when abnormal brain activity starts to emerge, but before any seizures begin. Paz hopes that by reducing inflammation in the thalamus during this time through drug treatments, she may be able to stop epilepsy from developing. So far, early efforts to treat the chronic inflammation with a drug in an animal model of traumatic brain injury have revealed promising results.
“Our goal is to prevent epilepsy before it starts, rather than trying to reverse the problem after it’s too late. If we treat a patient right after their initial injury, we can mitigate the chronic inflammation and reduce the likelihood that they develop epilepsy,” she said.
Treating Alzheimer’s Disease with Anti-Epilepsy Drugs
Epileptic activity can also occur in aging-related neurodegenerative diseases. For example, patients with Alzheimer’s disease are at increased risk of developing seizures.
Jorge Palop, PhD, assistant investigator, and Lennart Mucke, MD, director of the Gladstone Institute of Neurological Disease, have been unraveling intriguing links between epilepsy and Alzheimer’s disease. A recent clinical study that emerged from their research revealed epileptic activity in roughly 40% of Alzheimer patients tested. Led by staff scientist Keith Vossel, MD, the team of researchers used sophisticated technologies to detect “subclinical” epileptic activity (too subtle to be noticed on standard clinical exams) and showed that Alzheimer patients with such activity had a faster cognitive decline than those without.
“The faster decline in Alzheimer patients with epileptic activity is consistent with findings we previously obtained in animal models,” said Mucke. “We think that hyper-excitability in the brain contributes to cognitive deficits by inducing a remodeling and possibly even loss of neuronal connections. Blocking abnormal network activity might stop this disease-promoting process.”
Mucke’s team discovered that an FDA-approved anti-epileptic drug called levetiracetam suppressed abnormal brain activity and reversed memory loss in an animal model of Alzheimer’s disease. In collaboration with researchers at the University of California, San Francisco Memory and Aging Center, they are now conducting a clinical trial to test the drug’s efficacy in Alzheimer’s patients.
Improved Therapies Provide New Hope
As is true for many neurological disorders, better therapies are needed to treat epilepsy and related conditions. Many of the anti-epilepsy drugs currently available have severe side effects, and there are several types of intractable epilepsies that are resistant to all existing medications. Similarly, despite numerous clinical trials, there is no effective treatment to prevent, halt, or reverse Alzheimer’s disease. The therapeutic strategies that Paz, Mucke and others at Gladstone are exploring offer new hope to preserve and resurrect the harmony of the brain’s “orchestra."
Featured Experts
Support Discovery Science
Your gift to Gladstone will allow our researchers to pursue high-quality science, focus on disease, and train the next generation of scientific thought leaders.
Gladstone’s Scientific Highlights of 2025
Gladstone’s Scientific Highlights of 2025
From fundamental insights to translational advances, here’s how Gladstone researchers moved science forward in 2025.
Gladstone Experts Alzheimer’s Disease Autoimmune Diseases COVID-19 Neurological Disease Genomic Immunology Cardiovascular Disease Data Science and Biotechnology Infectious Disease Conklin LabScience in Seconds | The Thinking Microscope: Research Powered by an AI Brain
Science in Seconds | The Thinking Microscope: Research Powered by an AI Brain
In this video, Steve Finkbeiner and Jeremy Linsley showcase Gladstone’s groundbreaking “thinking microscope”—an AI-powered system that can design, conduct, and analyze experiments autonomously to uncover new insights into diseases like Alzheimer’s, Parkinson’s, and ALS.
Gladstone Experts ALS Alzheimer’s Disease Parkinson’s Disease Neurological Disease Finkbeiner Lab AI Big DataKaterina Akassoglou Receives Zenith Fellows Award to Advance Alzheimer’s Research
Katerina Akassoglou Receives Zenith Fellows Award to Advance Alzheimer’s Research
Akassoglou has opened doors to understanding how the blood protein fibrin is involved in Alzheimer’s and other neurodegenerative diseases.
Awards News Release Alzheimer’s Disease Center for Neurovascular Brain Immunology Akassoglou Lab