Gladstone NOW: The Campaign Join Us on the Journey✕

SAN FRANCISCO, CA—Researchers at the Gladstone Institutes and University of California, San Francisco have shown that a loss of cells in the retina is one of the earliest signs of frontotemporal dementia (FTD) in people with a genetic risk for the disorder—even before any changes appear in their behavior.
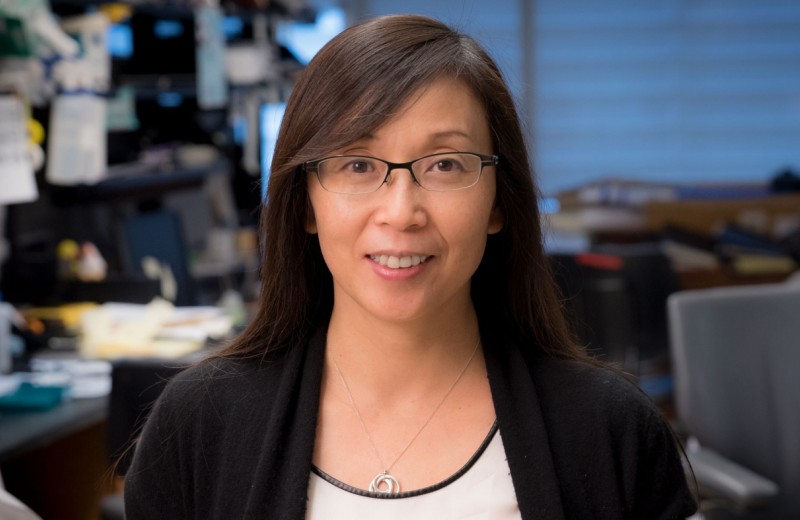
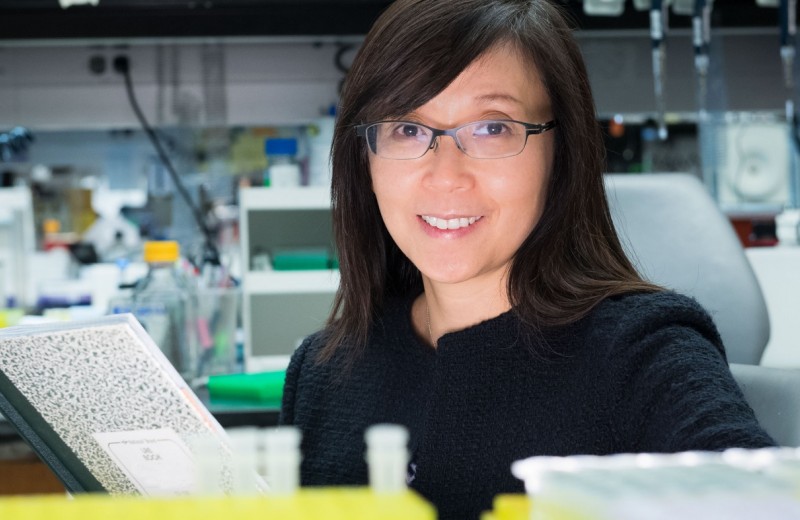
Published today in the Journal of Experimental Medicine, the researchers, led by Gladstone investigator Li Gan, PhD and UCSF associate professor of neurology Ari Green, MD, studied a group of individuals who had a certain genetic mutation that is known to result in FTD. They discovered that before any cognitive signs of dementia were present, these individuals showed a significant thinning of the retina compared with people who did not have the gene mutation.
“This finding suggests that the retina acts as a type of ‘window to the brain,’” said Dr. Gan. “Retinal degeneration was detectable in mutation carriers prior to the onset of cognitive symptoms, establishing retinal thinning as one of the earliest observable signs of familial FTD. This means that retinal thinning could be an easily measured outcome for clinical trials.”
![Retina cross-section from a healthy mouse showing TDP-43 staining (green), Ran staining (red), and nuclei (blue). [image: Michael Ward]](/sites/default/files/retina%20layers%20small%20%282%29.jpg?itok=HU8v0WzD) Retina cross-section from a healthy mouse showing TDP-43 staining (green), Ran staining (red), and nuclei (blue). [image: Michael Ward] Although it is located in the eye, the retina is made up of neurons with direct connections to the brain. This means that studying the retina is one of the easiest and most accessible ways to examine and track changes in neurons.
Retina cross-section from a healthy mouse showing TDP-43 staining (green), Ran staining (red), and nuclei (blue). [image: Michael Ward] Although it is located in the eye, the retina is made up of neurons with direct connections to the brain. This means that studying the retina is one of the easiest and most accessible ways to examine and track changes in neurons.
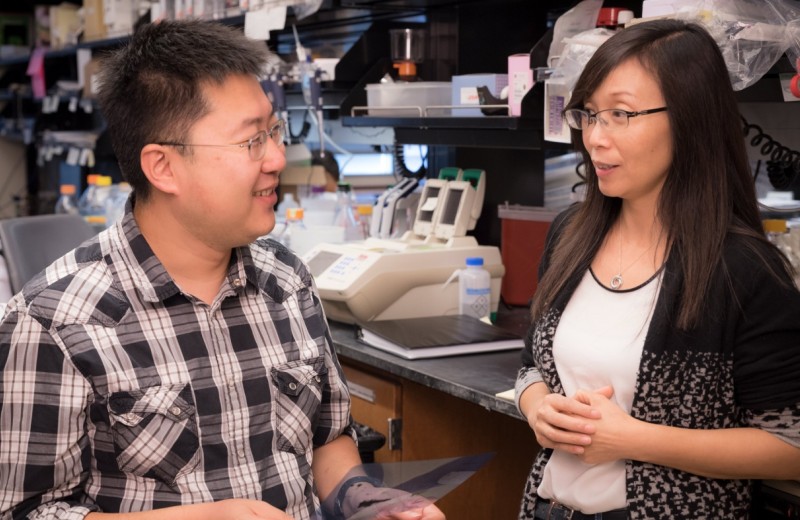
Lead author Michael Ward, MD, PhD, a postdoctoral fellow at the Gladstone Institutes and assistant professor of neurology at UCSF, explained, “The retina may be used as a model to study the development of FTD in neurons. If we follow these patients over time, we may be able to correlate a decline in retinal thickness with disease progression. In addition, we may be able to track the effectiveness of a treatment through a simple eye examination.”
The researchers also discovered new mechanisms by which cell death occurs in FTD. As with most complex neurological disorders, there are several changes in the brain that contribute to the development of FTD. In the inherited form researched in the current study, this includes a deficiency of the protein progranulin, which is tied to the mislocalization of another crucial protein, TDP-43, from the nucleus of the cell out to the cytoplasm.
However, the relationship between neurodegeneration, progranulin, and TDP-43 was previously unclear. In follow-up studies using a genetic mouse model of FTD, the scientists were able to investigate this connection for the first time in neurons from the retina. They identified a depletion of TDP-43 from the cell nuclei before any signs of neurodegeneration occurred, signifying that this loss may be a direct cause of the cell death associated with FTD.
TDP-43 levels were shown to be regulated by a third cellular protein called Ran. By increasing expression of Ran, the researchers were able to elevate TDP-43 levels in the nucleus of progranulin-deficient neurons and prevent their death.
“With these findings,” said Dr. Gan, “we now not only know that retinal thinning can act as a pre-symptomatic marker of dementia, but we’ve also gained an understanding into the underlying mechanisms of frontotemporal dementia that could potentially lead to novel therapeutic targets.”
This research was conducted in collaboration with scientists from the University of Alabama at Birmingham, and the University of Texas Southwestern. It was funded by the Consortium for Frontotemporal Dementia Research, Bluefield Project to Cure FTD, National Institutes of Health, UCSF Resource Allocation Program, UCSF Alzheimer’s Disease Research Center, Chartrand Foundation and Clinical & Science Translational Institute, Howard Hughes Medical Institute, Alzheimer’s Association, Welch Foundation, and Alzheimer’s Drug Discovery Foundation.
New Study Resolves Debate about How the Brain’s Immune Cells Regenerate
New Study Resolves Debate about How the Brain’s Immune Cells Regenerate
Gladstone scientists investigate how microglial cells maintain their population
News Release Research (Publication) Alzheimer’s Disease Neurological Disease Gan LabOne Copy of a Gene May Be Worse Than None at All
One Copy of a Gene May Be Worse Than None at All
A team of researchers shows that missing one copy of the TREM2 gene can exacerbate Alzheimer’s disease pathology
News Release Research (Publication) Alzheimer’s Disease Neurological Disease Gan Lab AgingGrowing Human Brain Cells in the Lab
Growing Human Brain Cells in the Lab
Scientists develop a cheaper, quicker, and more reliable stem cell–based technology to facilitate drug discovery
Gan Lab Stem Cells/iPSCs Alzheimer’s Disease