Gladstone NOW: The Campaign Join Us on the Journey✕
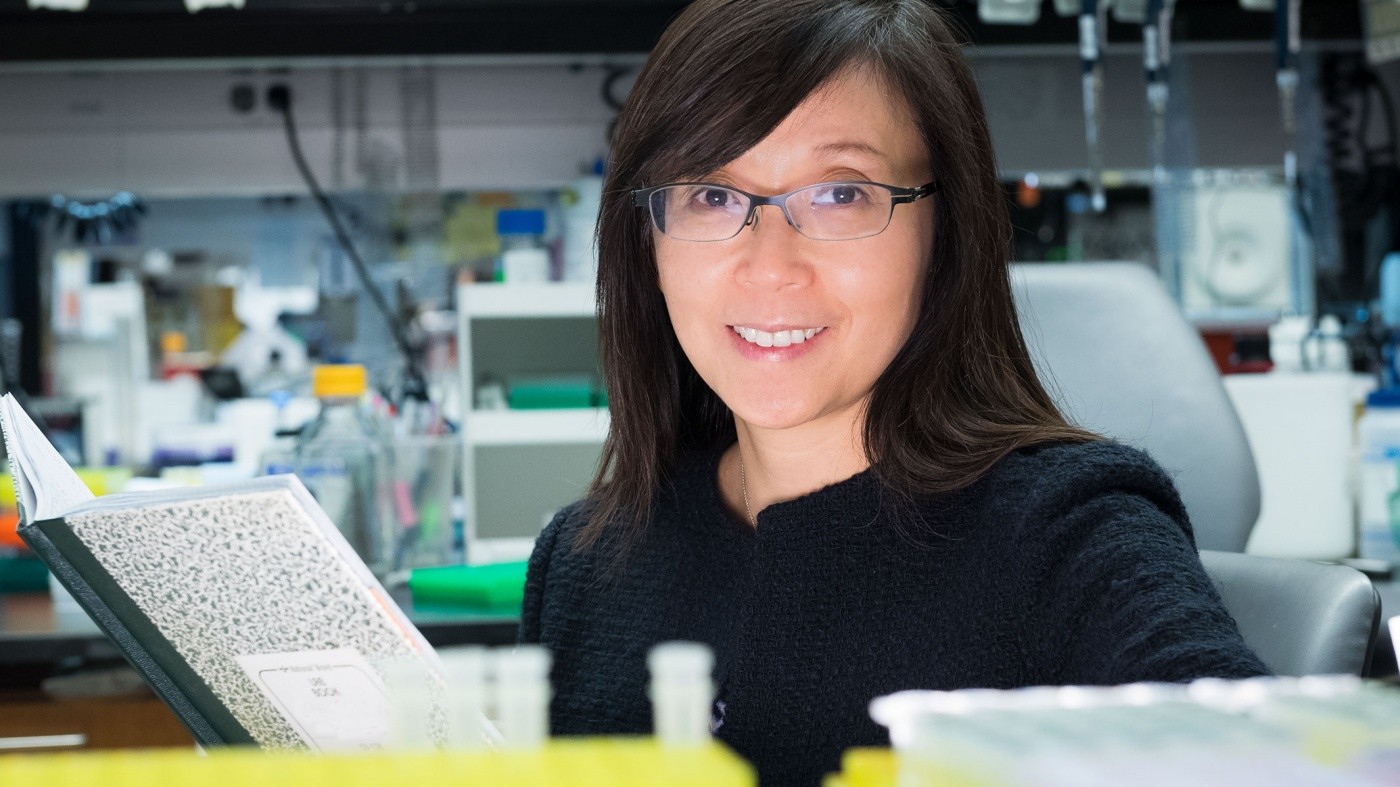
Li Gan and her team show that missing one copy of a gene called TREM2 can exacerbate Alzheimer’s disease pathology.
Late-onset Alzheimer’s disease is the most common form of dementia, and patients with one malfunctioning copy of a gene called TREM2 have a three-fold higher risk of developing the disease.
Of the two copies of the gene these patients inherit—one from each parent—one TREM2 gene is mutated, while the other is healthy. Surprisingly, a group of scientists at the Gladstone Institutes recently discovered that missing one functioning TREM2 gene is actually worse than having no TREM2 genes at all.
The team led by Senior Investigator Li Gan, PhD, conducted a study to uncover the role of TREM2 in Alzheimer’s disease. To do so, they examined mice that had two, one, or no TREM2 genes.
“We compared the three models to tease apart the function of TREM2 and we were stunned by the results,” said Gan. “We found that removing one TREM2 gene was actually more harmful than when we removed both.”
In their recent study published in the journal PNAS, researchers in Gan’s laboratory showed that partial loss of TREM2 has detrimental effects on the function of the brain’s immune cells and also increases inflammation and brain atrophy. In addition, they found that mice with only one TREM2 gene develop more tau pathology. Tau is one of the key pathogens that builds up in the brain of patients with Alzheimer’s disease.
Remarkably, the researchers noticed that a complete loss of TREM2 actually had protective benefits in a mouse model with tau aggregation.
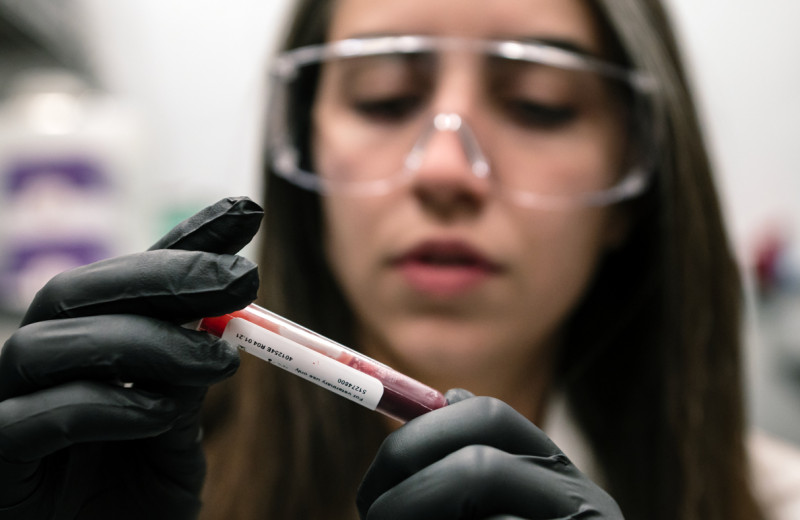
“Our findings indicate that strategies to lower levels of TREM2 could worsen rather than slow the progression of the disease,” said Faten Sayed, graduate student in Gan’s laboratory and first author of the study.
If the researchers had only looked at the effect of complete loss of TREM2, they might have concluded that blocking TREM2 would be therapeutic. But Gan’s results caution against such an approach.
“No drug could completely eliminate the function of TREM2, so trying to do so would only result in a partial loss of function, which might be more detrimental to the patient,” said Gan. “Our data also suggest that enhancing TREM2 could be beneficial against diseases associated with tau aggregation, which is contrary to what previous studies have implied.”
Another interesting fact about TREM2 is that it’s specific to immune cells in the brain. So, this study strongly supports human genetics evidence that links changes in innate immunity to Alzheimer's disease.
“Our paper provides valuable insight into how TREM2 controls the brain’s immune system, but we still don’t know how the disease-causing mutation in TREM2 works,” said Gan. “Our next steps will focus on gaining a deeper understanding of the gene mutation in the hopes of eventually identifying drug targets for neurodegenerative disease.”
The study was conducted in collaboration with Senior Investigator Katerina Akassoglou, as well as Maria Telpoukhovskaia, Lay Kodama, Yaqiao Li, Yungui Zhou, David Le, Axel Hauduc, Connor Ludwig, Claire Clelland, Lihong Zhan, and Dimitrios Davalos from Gladstone. Giovanni Coppola, Fuying Gao, and Yonatan A. Cooper from the UCLA Brain Research Institute also contributed. The Bioinformatics Core facility, the Genomics Core facility, and the Histology and Light Microscopy Core facility at Gladstone were also critical this study.
Research was supported by the National Institute of Aging, the National Institute of Neurological Diseases and Stroke, and the American Heart Association.
For Media
Julie Langelier
Associate Director, Communications
415.734.5000
Email
About Gladstone Institutes
Gladstone Institutes is an independent, nonprofit life science research organization that uses visionary science and technology to overcome disease. Established in 1979, it is located in the epicenter of biomedical and technological innovation, in the Mission Bay neighborhood of San Francisco. Gladstone has created a research model that disrupts how science is done, funds big ideas, and attracts the brightest minds.
Support Discovery Science
Your gift to Gladstone will allow our researchers to pursue high-quality science, focus on disease, and train the next generation of scientific thought leaders.
Gladstone Scientist Nadia Roan Elected to American Academy of Microbiology
Gladstone Scientist Nadia Roan Elected to American Academy of Microbiology
Roan has made great strides in understanding how persistent viruses including HIV cause disease and how immunity to viruses shapes human health.
Awards News Release COVID-19 HIV/AIDS Infectious Disease Roan LabRed Blood Cells Soak Up Sugar at High Altitude, Protecting Against Diabetes
Red Blood Cells Soak Up Sugar at High Altitude, Protecting Against Diabetes
New study shows red blood cells act as hidden glucose sponges in low-oxygen conditions, explaining why people living at high altitude have lower diabetes rates and pointing toward new treatments.
News Release Research (Publication) Diabetes Jain LabDisrupted Boundary Between Cell Types Linked to Common Heart Defects
Disrupted Boundary Between Cell Types Linked to Common Heart Defects
Gladstone scientists identified a cellular boundary that guides heart development and revealed how disrupting it can lead to holes in the heart’s wall.
News Release Research (Publication) Congenital Heart Disease Cardiovascular Disease Bruneau Lab