Gladstone NOW: The Campaign Join Us on the Journey✕
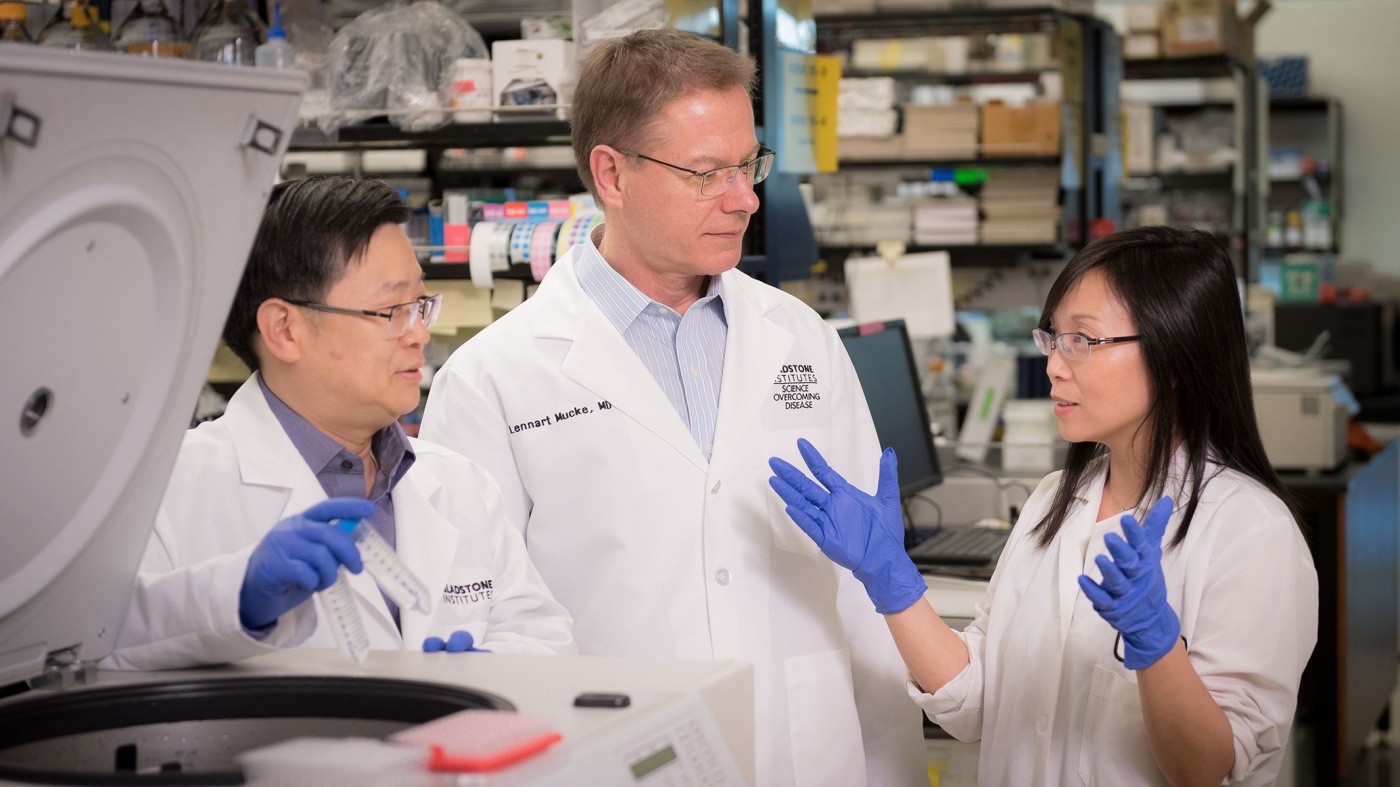
Yadong Huang, MD, PhD, Lennart Mucke, MD, and Li Gan, PhD, are taking a comprehensive approach to dementia research, pursuing several potential causal factors of the disease in the hopes of discovering breakthrough treatments. [Photo: Chris Goodfellow, Gladstone Institutes]
Some of the brightest minds in biology are working to solve one of the greatest challenges in medicine. Yet despite their best efforts, Alzheimer’s disease and other dementias continue to ravage aging populations across the globe.
An estimated 46 million people are afflicted by the disorders, and this number is expected to triple by 2050. Millions of hours and billions of dollars have been invested, but a cure or even an effective treatment for dementing diseases remains elusive. Time and again, clinical trials aimed to improve symptoms or delay cognitive decline have failed. Though experimental drugs show promising results in animal models of the disease, they have yet to be proven effective in patients.
There is also a disconnect between the multifactorial nature of the disease and the restrictive approach pharmaceutical companies have taken, investing almost exclusively in drugs aimed at the amyloid beta protein. For decades, the conventional wisdom has been that the build-up of amyloid plaques in the brain—ugly clumps of the protein that stick to the outside of neurons like old chewing gum on an alley wall—was at the root of the memory loss and behavioral changes characteristic of Alzheimer’s disease. However, although these plaques appear alarming, they are likely not the only cause of the disease.
A New Approach
Scientists at the Gladstone Institutes approach dementia as a complex condition with multiple genetic and biological causes, and therefore are investigating multiple ways to treat it.
“We already know there are several different types of dementia, such as Alzheimer’s disease, frontotemporal dementia, and dementia with Lewy bodies, and these conditions have disparate genetic and neurobiological contributors,” explained Lennart Mucke, MD, director of the Gladstone Institute of Neurological Disease. “Now we think there may also be several biological causes even within one disease like Alzheimer’s.”
Acknowledging the complexity of the condition, Gladstone researchers are investigating a suite of proteins involved in dementia, including tau, apoE4, klotho, adenosine receptors, and BRCA1, as well as amyloid beta. Working as an interdisciplinary team of scientists, clinicians, and industry partners, they hope that a comprehensive approach targeting many of these proteins will lead to better treatments for dementia.
The Protein Targets
Tau
Scientists have long known that the protein tau accumulates inside neurons in the brains of patients with Alzheimer’s disease. However, as the scientific field focused its efforts on the promise of amyloid beta, it largely passed over research into therapies addressing tau.
Recent discoveries have rekindled interest in tau as a major driver of dementia, and scientists at Gladstone are investigating ways to reduce levels of the protein as a potential treatment for dementia. Indeed, several studies have shown that decreasing tau prevents cell death and can restore cognitive function in animal models of Alzheimer’s disease. One exciting breakthrough by Gladstone senior investigator Li Gan, PhD, revealed that the drug salsalate—a variety of aspirin—can reverse memory loss in a mouse model of dementia by preventing tau from accumulating inside cells.
“We think tau is a critical contributor to dementia, but there are no drugs currently available that target the protein,” said Gan. “Salsalate’s effect on tau indicates that it could be a promising new therapeutic approach to treat dementia. Also, given that salsalate is a well-established and safe prescription drug, we believe it can have immediate clinical applications.”
A clinical trial testing salsalate’s effectiveness in treating neurodegenerative disease is currently underway.
ApoE4
Genetically, the E4 version of the apolipoprotein (apoE4) gene is the most important risk factor for Alzheimer’s disease. Over the past two decades, Gladstone president emeritus Robert Mahley, MD, PhD, and senior investigator Yadong Huang, MD, PhD, have worked to illuminate how the presence of apoE4 results in memory deficits. Their work indicates that the presence of the apoE4 protein leads to the loss of a particular type of brain cell called inhibitory interneurons, which in turn results in abnormal brain activity. The scientists are now researching several approaches, including cell therapy and drugs, to restore normal brain activity and reverse cognitive impairments in carriers of the apoE4 gene.
“We see significant dysfunction in the brains and behavior of apoE4 mice even when there is no accumulation of amyloid beta,” said Huang. “Our research suggests that the cognitive impairment is due to a change in neural activity that disrupts the consolidation of new memories. Discovering a way to normalize brain activity will be key in treating Alzheimer’s disease.”
Klotho
Rather than focusing solely on reversing cognitive decline, an alternative approach to improving dementia symptoms is to boost cognitive reserve. In a pair of studies, Mucke’s lab, together with collaborators from other institutions, discovered that a variant of the KLOTHO gene, which has previously been shown to increase longevity, is associated with improved cognitive function. What’s more, the scientists revealed that elevating levels of the klotho protein in a mouse model of Alzheimer’s disease protected the animals from the effects of amyloid accumulation. The researchers think this resistance to dysfunction stems from the beneficial effects of klotho on synapses—connections between brain cells, which are lost in Alzheimer’s disease. The next step is to identify and test drugs that can elevate klotho levels or mimic its effects on the brain.
Adenosine Receptors
Most research into cognition focuses on neurons. However, one recent Gladstone study suggested that astrocytes—support cells in the brain—may also play an important role in memory. The scientists discovered that reducing the number of receptors for the chemical adenosine on astrocytes improved memory in healthy mice. More notably, blocking this receptor prevented memory impairments in a mouse model of Alzheimer’s disease. These findings suggest that blocking adenosine receptors may offer a new approach to enhance memory and stave off memory decline in Alzheimer’s disease. Because such drugs have already been developed for Parkinson’s disease, a repurposing trial for Alzheimer’s disease will likely be initiated in the near future.
BRCA1
In perhaps the most surprising revelation, Gladstone researchers found a connection between BRCA1 and dementia. Mutations in the BRCA1 gene, which produces a protein of the same name, are most commonly associated with breast cancer. In the brain, the BRCA1 protein helps repair DNA double-strand breaks that can occur in neurons from increased cellular activity. However, in Alzheimer’s disease, there is a depletion of BRCA1 in neurons, most likely as a result of amyloid beta accumulation. Research in mouse models suggests that this depletion results in an imbalance between DNA damage and repair, and contributes to neurodegeneration and cognitive decline. The scientists are now testing whether increasing BRCA1 protein levels in the brain can prevent or reverse dysfunction.
Multi-factorial Treatments for a Multi-faceted Disorder
Gladstone scientists do not limit themselves to one field of thought, which increases their chances of making an unexpected breakthrough. For a complex multifactorial disorder like dementia, this mindset and multipronged approach are especially critical.
“Dementia is a complicated, multi-faceted condition,” said Mucke. “Pursuing a host of different treatment options that tackle diverse proteins implicated in dementing diseases is a logical approach to solving the problem. By discovering the biological underpinnings of these diseases, we may be able to not only treat patients’ symptoms, but also eradicate the root causes.”
Want to Join the Team?
Our people are our most important asset. We offer a wide array of career opportunities both in our administrative offices and in our labs.
Explore CareersGladstone’s Scientific Highlights of 2025
Gladstone’s Scientific Highlights of 2025
From fundamental insights to translational advances, here’s how Gladstone researchers moved science forward in 2025.
Gladstone Experts Alzheimer’s Disease Autoimmune Diseases COVID-19 Neurological Disease Genomic Immunology Cardiovascular Disease Data Science and Biotechnology Infectious Disease Conklin LabScience in Seconds | The Thinking Microscope: Research Powered by an AI Brain
Science in Seconds | The Thinking Microscope: Research Powered by an AI Brain
In this video, Steve Finkbeiner and Jeremy Linsley showcase Gladstone’s groundbreaking “thinking microscope”—an AI-powered system that can design, conduct, and analyze experiments autonomously to uncover new insights into diseases like Alzheimer’s, Parkinson’s, and ALS.
Gladstone Experts ALS Alzheimer’s Disease Parkinson’s Disease Neurological Disease Finkbeiner Lab AI Big DataKaterina Akassoglou Receives Zenith Fellows Award to Advance Alzheimer’s Research
Katerina Akassoglou Receives Zenith Fellows Award to Advance Alzheimer’s Research
Akassoglou has opened doors to understanding how the blood protein fibrin is involved in Alzheimer’s and other neurodegenerative diseases.
Awards News Release Alzheimer’s Disease Center for Neurovascular Brain Immunology Akassoglou Lab