Gladstone NOW: The Campaign Join Us on the Journey✕

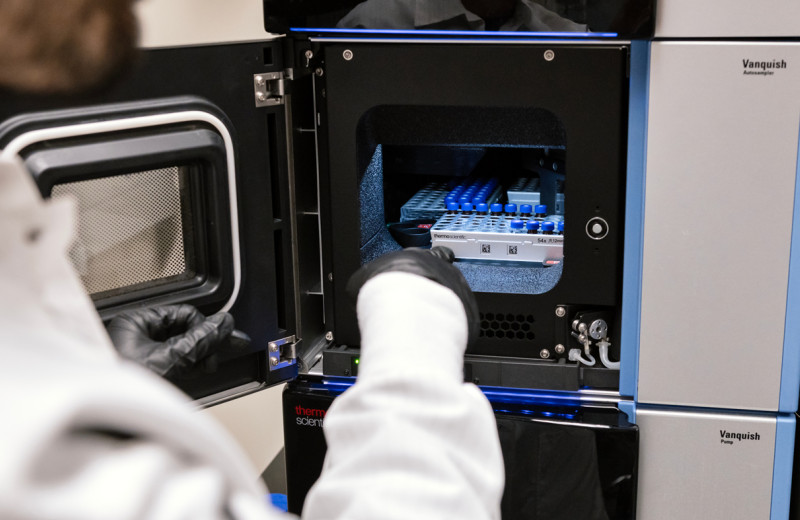
Bruce Conklin (left) and Beeke Wienert (right) were part of a team that developed a new technique, named DISCOVER-Seq, to identify off-target damage caused by CRISPR genome editing.
Since the CRISPR genome editing technology was invented in 2012, it has shown great promise to treat a number of intractable diseases. However, scientists have struggled to identify potential off-target effects in therapeutically relevant cell types, which remains the main barrier to moving therapies to the clinic. Now, a group of scientists at the Gladstone Institutes and the Innovative Genomics Institute (IGI), with collaborators at AstraZeneca, have developed a reliable method to do just that.
CRISPR edits a person’s genome by cutting the DNA at a specific location. The challenge is to ensure the tool doesn’t also make cuts elsewhere along the DNA—damage referred to as “off-target effects,” which could have unforeseen consequences.
In a study published in the journal Science, the two first authors, Beeke Wienert and Stacia Wyman, found a new way to approach the problem.
“The human genome is extremely large—if you printed the entire DNA sequence, you would end up with a novel as tall as a 16-story building.”
“When CRISPR makes a cut, the DNA is broken,” says Wienert, PhD, who began the work in Jacob E. Corn’s IGI laboratory and who is now a postdoctoral scholar in Bruce R. Conklin’s laboratory at Gladstone. “So, in order to survive, the cell recruits many different DNA repair factors to that particular site in the genome to fix the break and join the cut ends back together. We thought that if we could find the locations of these DNA repair factors, we could identify the sites that have been cut by CRISPR.”
To test their idea, the researchers studied a panel of different DNA repair factors. They found that one of them, called MRE11, is one of the first responders to the site of the cut. Using MRE11, the scientists developed a new technique, named DISCOVER-Seq, that can identify the exact sites in the genome where a cut has been made by CRISPR.
“The human genome is extremely large—if you printed the entire DNA sequence, you would end up with a novel as tall as a 16-story building,” explains Conklin, MD, senior investigator at Gladstone and deputy director at IGI. “When we want to cut DNA with CRISPR, it’s like we’re trying to remove one specific word on a particular page in that novel.”
“You can think of the DNA repair factors as different types of bookmarks added to the book,” Conklin adds. “While some may bookmark an entire chapter, MRE11 is a bookmark that drills down to the exact letter than has been changed.”
Different methods currently exist to detect CRISPR off-target effects. However, they come with limitations that range from producing false-positive results to killing the cells they’re examining. In addition, the most common method used to date is currently limited to cultured cells in the laboratory, excluding its use in patient-derived stem cells or animal tissue.
“Because our method relies on the cell’s natural repair process to identify cuts, it has proven to be much less invasive and much more reliable,” says Corn, PhD, who now runs a laboratory at ETH Zurich. “We were able to test our new DISCOVER-Seq method in induced pluripotent stem cells, patient cells, and mice, and our findings indicate that this method could potentially be used in any system, rather than just in the lab.”
The DISCOVER-Seq method, by being applied to new cell types and systems, has also revealed new insights into the mechanisms used by CRISPR to edit the genome, which will lead to a better understanding of the biology of how this tool works.
“The new method greatly simplifies the process of identifying off-target effects while also increasing the accuracy of the results,” says Conklin, who is also a professor of medical genetics and molecular pharmacology at UC San Francisco (UCSF). “This could allow us to better predict how genome editing would work in a clinical setting. As a result, it represents an essential step in improving pre-clinical studies and bringing CRISPR-based therapies closer to the patients in need.”
Gladstone’s Hannah L. Watry and Luke M. Judge (who is also at UCSF) contributed to this study. Other authors also include Christopher D. Richardson, Jonathan T. Vu, and Katelynn R. Kazane from IGI, Charles D. Yeh from ETH Zurich, as well as Pinar Akcakaya, Michelle J. Porritt, and Michaela Morlock from AstraZeneca.
The work was supported by Gladstone, the National Institutes of Health (grants EY028249 and HL13535801), the Li Ka Shing Foundation, the Heritage Medical Research Institute, the Fanconi Anemia Research Foundation, a Sir Keith Murdoch Fellowship from the American Australian Association, and an Early Career Fellowship from the National Health and Medical Research Council.
For Media
Julie Langelier
Associate Director, Communications
415.734.5000
Email
About Gladstone Institutes
Gladstone Institutes is an independent, nonprofit life science research organization that uses visionary science and technology to overcome disease. Established in 1979, it is located in the epicenter of biomedical and technological innovation, in the Mission Bay neighborhood of San Francisco. Gladstone has created a research model that disrupts how science is done, funds big ideas, and attracts the brightest minds.
Featured Experts
Support Discovery Science
Your gift to Gladstone will allow our researchers to pursue high-quality science, focus on disease, and train the next generation of scientific thought leaders.
New Tool Reveals the Secrets of HIV-Infected Cells
New Tool Reveals the Secrets of HIV-Infected Cells
Developed by Gladstone scientists, HIV-seq could uncover new opportunities for treating HIV.
News Release Research (Publication) HIV/AIDS Infectious Disease Roan LabVitamin B3 Therapy Offers Hope for Fatal Childhood Disease
Vitamin B3 Therapy Offers Hope for Fatal Childhood Disease
A new framework that matches vitamins with genetic diseases helped uncover that high-dose vitamin B3 can dramatically extend survival in mice with NAXD deficiency.
News Release Research (Publication) Rare Diseases Jain LabGladstone Scientist Nadia Roan Elected to American Academy of Microbiology
Gladstone Scientist Nadia Roan Elected to American Academy of Microbiology
Roan has made great strides in understanding how persistent viruses including HIV cause disease and how immunity to viruses shapes human health.
Awards News Release COVID-19 HIV/AIDS Infectious Disease Roan Lab