Gladstone NOW: The Campaign Join Us on the Journey✕

Sean Whalen (left), Katie Pollard (right), and their colleagues discover that many changes to the genomes of early humans had opposing effects from each other, possibly because of a delicate balance between improved cognition and psychiatric disease risk.
Humans and chimpanzees differ in only one percent of their DNA. Human accelerated regions (HARs) are parts of the genome with an unexpected amount of these differences. HARs were stable in mammals for millennia but quickly changed in early humans. Scientists have long wondered why these bits of DNA changed so much, and how the variations set humans apart from other primates.
Now, researchers at Gladstone Institutes have analyzed thousands of human and chimpanzee HARs and discovered that many of the changes that accumulated during human evolution had opposing effects from each other.
“This helps answer a longstanding question about why HARs evolved so quickly after being frozen for millions of years,” says Katie Pollard, PhD, director of the Gladstone Institute of Data Science and Biotechnology and lead author of the new study published today in Neuron. “An initial variation in a HAR might have turned up its activity too much, and then it needed to be turned down.”
The findings, she says, have implications for understanding human evolution. In addition—because she and her team discovered that many HARs play roles in brain development—the study suggests that variations in human HARs could predispose people to psychiatric disease.
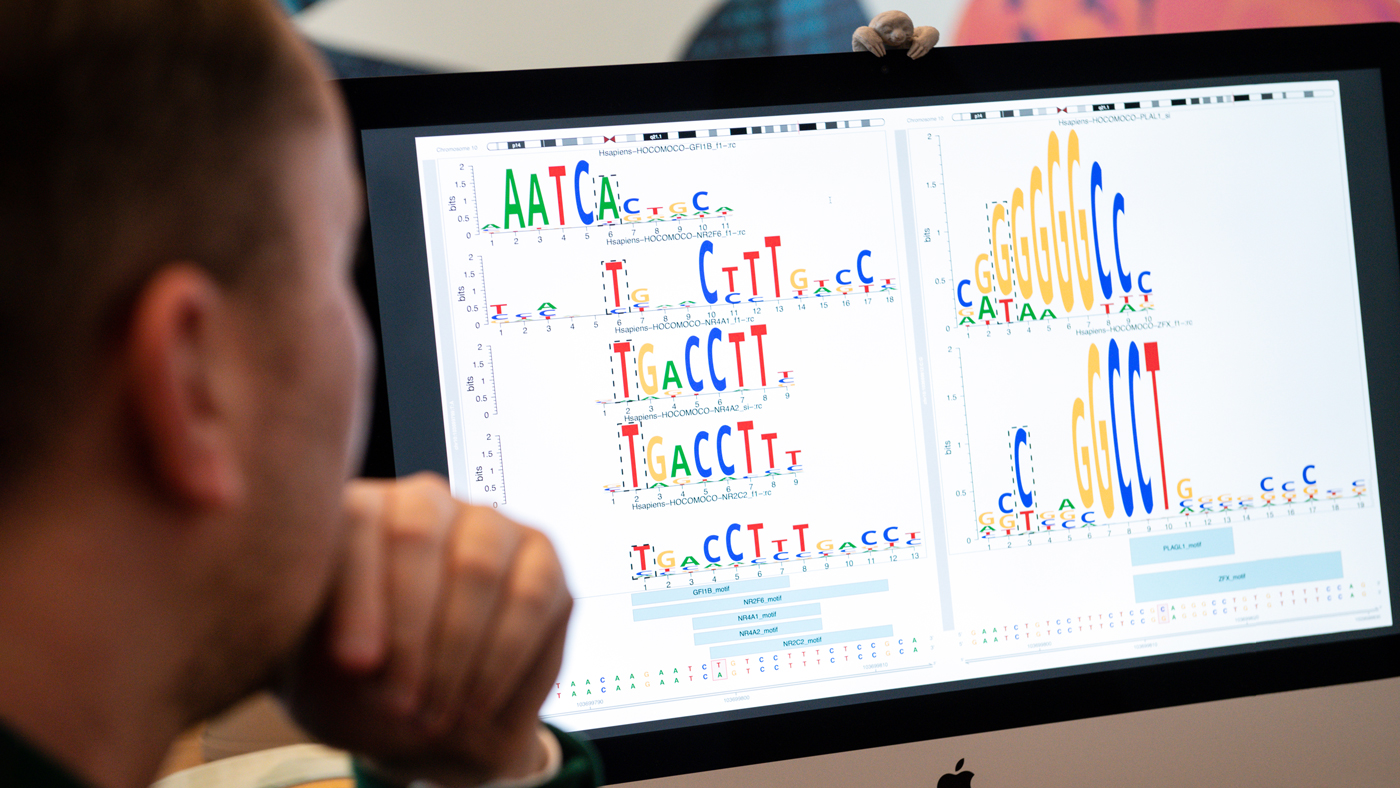
“These results required cutting-edge machine learning tools to integrate dozens of novel datasets generated by our team, providing a new lens to examine the evolution of HAR variants,” says Sean Whalen, PhD, first author of the study and senior staff research scientist in Pollard’s lab.
Enabled by Machine Learning
Pollard discovered HARs in 2006 when comparing the human and chimpanzee genomes. While these stretches of DNA are nearly identical among all humans, they differ between humans and other mammals. Pollard’s lab went on to show that the vast majority of HARs are not genes, but enhancers— regulatory regions of the genome that control the activity of genes.
More recently, Pollard’s group wanted to study how human HARs differ from chimpanzee HARs in their enhancer function. In the past, this would have required testing HARs one at a time in mice, using a system that stains tissues when a HAR is active.
Instead, Whalen input hundreds of known human brain enhancers, and hundreds of other non-enhancer sequences, into a computer program so that it could identify patterns that predicted whether any given stretch of DNA was an enhancer. Then he used the model to predict that a third of HARs control brain development.
“Basically, the computer was able to learn the signatures of brain enhancers,” says Whalen.
Whalen and his fellow scientists found that nearly half of HARs contain two or more variants with large opposing effects, mimicking what the machine learning algorithms had predicted.
Knowing that each HAR has multiple differences between humans and chimpanzees, Pollard and her team questioned how individual variants in a HAR impacted its enhancer strength. For instance, if eight nucleotides of DNA differed between a chimpanzee and human HAR, did all eight have the same effect, either making the enhancer stronger or weaker?
“We’ve wondered for a long time if all the variants in HARs were required for it to function differently in humans, or if some changes were just hitchhiking along for the ride with more important ones,” says Pollard, who is also chief of the division of bioinformatics in the Department of Epidemiology and Biostatistics at UC San Francisco (UCSF), as well as a Chan Zuckerberg Biohub investigator.
To test this, Whalen applied a second machine learning model, which was originally designed to determine if DNA differences from person to person affect enhancer activity. The computer predicted that 43 percent of HARs contain two or more variants with large opposing effects: some variants in a given HAR made it a stronger enhancer, while other changes made the HAR a weaker enhancer.
This result surprised the team, who had expected that all changes would push the enhancer in the same direction, or that some “hitchhiker” changes would have no impact on the enhancer at all.
Measuring HAR Strength
To validate this compelling prediction, Pollard collaborated with the laboratories of Nadav Ahituv, PhD, and Alex Pollen, PhD, at UCSF. The researchers fused each HAR to a small DNA barcode. Each time a HAR was active, enhancing the expression of a gene, the barcode was transcribed into a piece of RNA. Then, the researchers used RNA sequencing technology to analyze how much of that barcode was present in any cell—indicating how active the HAR had been in that cell.
“This method is much more quantitative because we have exact barcode counts instead of microscopy images,” says Ahituv. “It’s also much higher throughput; we can look at hundreds of HARs in a single experiment.”
“We can never wind the clock back and know exactly what happened in evolution. But we can simulate what might have happened and identify which DNA changes are most likely to explain unique aspects of the human brain, including its propensity for psychiatric disease.”
When the group carried out their lab experiments on over 700 HARs in precursors to human and chimpanzee brain cells, the data mimicked what the machine learning algorithms had predicted.
“We might not have discovered human HAR variants with opposing effects at all if the machine learning model hadn’t produced these startling predictions,” said Pollard.
Implications for Understanding Psychiatric Disease
The idea that HAR variants played tug-of-war over enhancer levels fits in well with a theory that has already been proposed about human evolution: that the advanced cognition in our species is also what has given us psychiatric diseases.
“What this kind of pattern indicates is something called compensatory evolution,” says Pollard. “A large change was made in an enhancer, but maybe it was too much and led to harmful side effects, so the change was tuned back down over time—that’s why we see opposing effects.”

By better understanding HARs, Pollard (left)—in conversation here with Whalen (right)—hopes her research might eventually help shed light on new treatments for psychiatric diseases.
If initial changes to HARs led to increased cognition, perhaps subsequent compensatory changes helped tune back down the risk of psychiatric diseases, Pollard speculates. Her data, she adds, can’t directly prove or disprove that idea. But in the future, a better understanding of how HARs contribute to psychiatric disease could not only shed light on evolution, but on new treatments for these diseases.
“We can never wind the clock back and know exactly what happened in evolution,” says Pollard. “But we can use all these scientific techniques to simulate what might have happened and identify which DNA changes are most likely to explain unique aspects of the human brain, including its propensity for psychiatric disease.”
For Media
Julie Langelier
Associate Director, Communications
415.734.5000
Email
About the Study
The paper “Machine learning dissection of human accelerated regions in primate neurodevelopment,” was published in the journal Neuron on January 13, 2023.
Other authors are Kathleen Keough, Alex Williams, Md. Abu Hassan Samee, and Sean Thomas of Gladstone; Fumitaka Inoue, Hane Ryu, Tyler Fair, Eirene Markenscoff-Papadimitrious, Beatriz Alvarado, Orry Elor, Dianne Laboy Cintron, Erik Ullian, Arnold Kriegstein, and John Rubenstein of UC San Francisco; Martin Kircher, Beth Martin, and Jay Shendure of University of Washington; and Robert Krencik of Houston Methodist Research Institute.
The work was supported by the Schmidt Futures Foundation and the National Institutes of Health (DP2MH122400-01, R35NS097305, FHG011569A, R01MH109907, U01MH116438, UM1HG009408, UM1HG011966, 2R01NS099099).
About Gladstone Institutes
Gladstone Institutes is an independent, nonprofit life science research organization that uses visionary science and technology to overcome disease. Established in 1979, it is located in the epicenter of biomedical and technological innovation, in the Mission Bay neighborhood of San Francisco. Gladstone has created a research model that disrupts how science is done, funds big ideas, and attracts the brightest minds.
Want to Join the Team?
Our people are our most important asset. We offer a wide array of career opportunities both in our administrative offices and in our labs.
Explore CareersDisrupted Boundary Between Cell Types Linked to Common Heart Defects
Disrupted Boundary Between Cell Types Linked to Common Heart Defects
Gladstone scientists identified a cellular boundary that guides heart development and revealed how disrupting it can lead to holes in the heart’s wall.
News Release Research (Publication) Congenital Heart Disease Cardiovascular Disease Bruneau LabGene Editing Strategy Could Treat Hundreds of Inherited Diseases More Effectively
Gene Editing Strategy Could Treat Hundreds of Inherited Diseases More Effectively
Scientists at Gladstone show the new method could treat the majority of patients with Charcot-Marie-Tooth disease.
News Release Research (Publication) Neurological Disease Conklin Lab CRISPR/Gene EditingGenomic Maps Untangle the Complex Roots of Disease
Genomic Maps Untangle the Complex Roots of Disease
Findings of the new study in Nature could streamline scientific discovery and accelerate drug development.
News Release Research (Publication) Marson Lab Genomics Genomic Immunology




