Gladstone NOW: The Campaign Join Us on the Journey✕

Gordon Keller, winner of the 2019 Ogawa-Yamanaka Stem Cell Prize, realized early on the potential of embryonic stem cells.
Gordon Keller, PhD, was awarded the 2019 Ogawa-Yamanaka Stem Cell Prize for his research revealing how to efficiently guide pluripotent stem cells into multiple types of specialized cells. He is a senior scientist at the Princess Margaret Cancer Centre, director of the McEwen Stem Cell Institute at the University Health Network in Toronto, and professor of medical biophysics at the University of Toronto.
Keller discusses what it’s been like to watch stem cell research evolve over the more than three decades he’s been a part of the field.
The earliest stages of human embryonic development are marked by expansion, from a fertilized egg to hundreds of cells in a matter of days. As cells amass, they begin to specialize, taking on distinct forms and functions. The early days of stem cell science were like this too: a few researchers delving into the basic biology of stem cells, and then a seemingly exponential growth of interest—and countless new, specialized directions for research—as the implications for human health became clear.
Gordon Keller started studying stem cells in the early 1980s with only an inkling of the promise that these cells may hold. He was originally captivated by the fact that stem cells found in the bone marrow, so-called hematopoietic stem cells (HSCs), could generate diverse types of blood and immune cells. He developed strategies to label individual HSCs and track the different types of blood cells they are able to generate. At this time, he also became interested in working with stem cells found in embryos, so-called embryonic stem cells (ESCs), and exploring the molecular cues that led them down different developmental pathways when cultured in the lab.
By the time Shinya Yamanaka, MD, PhD, engineered induced pluripotent stem cells (iPSCs) in 2006, Keller was identifying the role of specific signaling molecules in coaxing ESCs to become specialized cells. His findings laid the groundwork for researchers to begin to turn Yamanaka’s iPSCs—a limitless source of stem cells—into different functional cell types.
That collection of work—spanning decades and covering numerous cell types—has now earned Keller the 2019 Ogawa-Yamanaka Stem Cell Prize. The prize is named in part after Yamanaka, a senior investigator at Gladstone Institutes, and was established in 2015 by the late Hiro and Betty Ogawa.
“I am very pleased that Gordon is the recipient of this year’s prize,” said Yamanaka, who is also director of Kyoto University's Center for iPS Cell Research and Application (CiRA). “His work has been essential for many scientists around the world, as he showed us how to differentiate stem cells into specific cell types.”
“Gordon was an obvious candidate for this prize, given his remarkable contributions to stem cell research and his interest in advancing the field toward clinical applications,” said Gladstone President Deepak Srivastava, MD, chair of the selection committee and director of the Roddenberry Stem Cell Center at Gladstone, who also serves as this year’s president of the International Society for Stem Cell Research.
The Development of a Career
The cues that guide stem cells down distinct developmental pathways—spurring them to differentiate into heart or brain or blood cells—are precise and reproducible. Keller’s own path, though, is somewhat more happenstance; he can’t pinpoint all the exact factors that drew him to study stem cells.
“I grew up on a farm in the middle of Canada,” said Keller. “The opportunities in those days were considerably more limited than they are today. I attended the local university, the University of Saskatchewan, and gravitated to the biological sciences as I always had a desire to understand the fundamentals of how things work.”
He followed his undergraduate degree with a graduate degree in immunology at the University of Alberta. It was during his postdoctoral fellowship at the Ontario Cancer Institute—where Ernest McCulloch and James Till had first discovered HSCs in the 1960s—that Keller first became interested in stem cells.

Gordon Keller presented his award-winning research at the 2019 Ogawa-Yamanaka Stem Cell Prize ceremony.
While stem cells can differentiate into many types of cells, the process isn’t instantaneous—it takes time and many developmental steps. In the 1980s, when Keller started studying stem cells, scientists were still figuring out what these steps were—along with all the intermediaries between a stem cell and a mature cell. Following his postdoctoral fellowship, Keller moved to Europe and took a position at the Basel Institute for Immunology in Switzerland. During this time, he worked on a new strategy to genetically label HSCs in the bone marrow. This allowed him to follow their developmental progression as new cells generated in the bone marrow would each carry the same genetic label as their parent stem cell.
Using this approach, Keller showed that myeloid and lymphoid cells—two different lineages of blood cells—came from the same HSC. But at the same time he was perfecting these techniques on HSCs, Keller learned about a new type of stem cell, just discovered in mice.
“I remember clearly, in 1984, when I heard Rolf Kemler give a talk about embryonic stem cells,” says Keller. “I was fascinated by the concept that these stem cells, over a period of time, could form all these other cell types in a Petri dish,” Keller adds, referring to the shallow dishes in which scientists typically grow cells in the lab.
Where HSCs could only give rise to blood and immune cells, mouse ESCs could differentiate into nearly every type of cell in the body—they were, as scientists called them, “pluripotent”. By the time he launched his own lab in the US, Keller had decided he wanted to focus his energy on mouse ESCs. Whether such pluripotent stem cells could be isolated from human embryos could only be theorized about at the time.
“It was a gamble to start working on mouse ESC-differentiation some 30 years ago because there was no guarantee we would ever have human stem cells to work with,” Keller says.
The gamble, though, paid off. In 1998, researchers isolated human embryonic stem cells (hESCs) for the first time.
“There were maybe a handful of labs working with mouse ESCs, trying to make different cell types in the dish. The interest in the general scientific community was fairly modest,” said Keller. “And then when James Thomson identified hESCs, it changed almost overnight. Because suddenly, there was a link to potential therapeutics and studying human biology in a dish.”
Mimicking the Precision of Development
Keller’s initial attempts at differentiating mouse ESCs into different cell types had been hit-or-miss. “It was tough work because there was no literature, there was no field,” he says. “At first, we would just try different conditions and wait and watch for our desired cell type, whether it was a red blood cell or a few beating heart muscle cells.”
Even with the slow progress, Keller worked out protocols for differentiating ESCs and identifying molecules that played key roles in this process—first in mouse and later in human cell cultures. But he also realized that there was a better way than trial-and-error to approach the problem of how to guide the cells’ differentiation. In fact, there was already a model system where pluripotent cells were able to differentiate into every cell type found in an adult—the embryo. If scientists could pinpoint exactly what was occurring in embryos as the different cell types and tissue developed, they could mimic that in the lab, Keller reasoned. So the first challenge was to understand how the many different functional cells were generated during the development of embryos.
“I came to the realization that this wasn’t a stem cell problem; it was a developmental biology problem,” said Keller. “Once I understood that, it became very exciting to follow the developmental progression of whatever lineage we studied, and we studied many over the years.”
In 1997, Keller’s team became the first to isolate hemangioblasts. These intermediaries between ESCs and mature blood can differentiate into both blood cells and the cells that make up the body’s blood vessels. The existence of a hemangioblast had been hypothesized many years earlier. Keller’s group went on to identify what molecules were necessary to direct hemangioblasts down each developmental lineage. Fortunately, the field of developmental biology was exploding at that time, revealing the key events dictating cell fate decisions in the embryo for most cell types, knowledge that fueled progress in stem cell biology.
During the early to mid-2000s, Keller’s group studied the roles of proteins known as cytokines that promote various differentiation pathways during development. This alphabet soup of molecules that includes Wnts, Notch, BMPs, TGF-β, and activin are familiar to most stem cell scientists today. Keller discovered that even minute differences in the levels of a cytokine can drastically affect the fate of a stem cell. Such differences reflect gradients of molecules found in a developing embryo—cells in one area of an embryo are destined to become a different type of cell than those in another area because they are exposed to different amounts or different combinations of cytokines.
“It can seem subtle to an experimenter in the lab,” says Keller. “While you’re pipetting at the bench, it may not seem that important to add one amount of a factor versus another, but the outcome can be remarkably different.”
Today, Keller still expresses amazement that the complexity of developmental biology can be mimicked in the Petri dish. “That it works as well as it does, I think, is truly remarkable,” he says. “We can make a billion heart cells, or a billion blood cells, and it works every time.”
At one point, Keller’s group was simultaneously studying the development of blood, heart, liver, and pancreas cells. Working with mouse and human ESCs, the researchers detailed what was occurring at a molecular level as these cells differentiated into each tissue type. It led to protocols for generating new cells—something of basic science interest but also, hopefully, eventual therapeutic application.
“Understanding how each of these cell types was made from the pluripotent stem cell was very exciting and something that I’m very proud of,” he says.
But Keller also points out that his work was a steady slog of tough experimentation. “There’s no one experiment that says ‘Eureka!’ but when you put the collection together, it clicks and you say ‘Aha! We have it. We understand this.’”
Moving toward the Clinic
By the early 2000s, although Keller had shown how to generate different cell types from human ESCs, moving these discoveries to patients was challenging because of ethical, legal, and funding issues. In 2006, though, Yamanaka’s announcement of iPSCs—stem cells that had been generated by turning back the clock on adult tissues—offered a new avenue for clinical experimentation.
“It completely opened the field to where you could imagine not only cellular therapeutics but also personalized medicine, disease modeling, and drug screening,” says Keller.
The big advantage of iPSCs is that they are patient-specific. Skin or blood cells can be collected from a patient, turned into iPSCs and then coaxed down a developmental pathway to generate personalized heart or brain or liver cells. To do that, scientists rely on the molecular cues that Keller and others discovered over decades of work with embryos and ESCs.
“Gordon’s work on differentiating ESCs laid the foundation for the success of iPSCs,” said George Daley, MD, PhD, dean of Harvard Medical School, and member of the award selection committee. “By the time iPSCs came along, he had assembled an enormous trove of knowledge for how to turn them into many types of cells; thereafter, applications of iPSCs to medical research took off.”

Deepak Srivastava, Deborah Sweet, and Shinya Yamanaka present the 2019 Ogawa-Yamanaka Stem Cell Prize to Gordon Keller.
In 2016, buoyed by the potential for applying his long-standing work in generating blood and heart cells to new iPSC science, Keller joined three other scientists, along with pharma giant Bayer AG and leading health-care investment firm Versant Ventures, to co-found BlueRock Therapeutics with one of the largest initial financings ever seen at that time in the history of the biotechnology sector. The company’s mission is to create a new generation of cellular medicines to reverse devastating diseases. Among their first projects are treatments for Parkinson’s disease and—based in part on Keller’s work—heart attacks.
Already, Keller and his colleagues have differentiated stem cells into cardiomyocytes, the muscle cells found in the heart. “The goal would be to introduce these cells into a patient who has had a heart attack and have these cells make new muscle in place of what would otherwise be scar tissue,” explains Keller.
Even as Keller immerses himself in helping shape BlueRock—he’s now officially a scientific adviser for the company—he says he still finds time for lab work.
“Even after thirty odd years, I try to go into the lab and look at cells every day,” he says. “It keeps me in touch and grounded as to why we’re doing what we’re doing.”
A Sculptor of Modern Regenerative Medicine
A Sculptor of Modern Regenerative Medicine
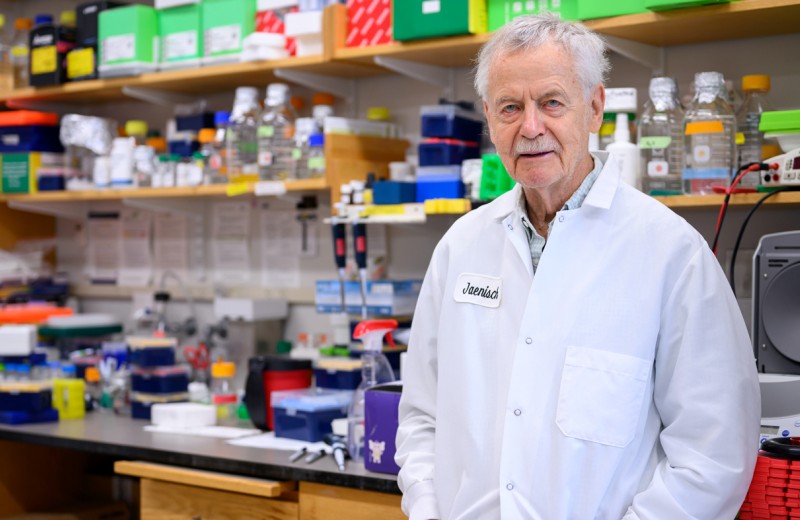
Among his myriad accomplishments, Rudolf Jaenisch—winner of the 2025 Ogawa-Yamanaka Stem Cell Prize—was the first to demonstrate the potential of induced pluripotent stem cells to treat disease.
Awards Ogawa Stem Cell Prize Profile Regenerative Medicine Stem Cells/iPSCsThe 2025 Ogawa-Yamanaka Stem Cell Prize Awarded to Rudolf Jaenisch
The 2025 Ogawa-Yamanaka Stem Cell Prize Awarded to Rudolf Jaenisch
Jaenisch is recognized for his trailblazing contributions to epigenetics and stem cell biology, which have shaped modern regenerative medicine.
Awards News Release Ogawa Stem Cell Prize Stem Cells/iPSCs2024 Ogawa-Yamanaka Stem Cell Prize Ceremony | Honoring Rusty Gage
2024 Ogawa-Yamanaka Stem Cell Prize Ceremony | Honoring Rusty Gage
Rewatch the 2024 Ogawa-Yamanaka Stem Cell Prize Ceremony, honoring 2024 recipient Rusty Gage.
Ogawa Stem Cell Prize