Gladstone NOW: The Campaign Join Us on the Journey✕

SAN FRANCISCO, CA—Scientists at the Gladstone Institutes have identified a novel mechanism by which a type of low-carb, low-calorie diet—called a “ketogenic diet”—could delay the effects of aging. This fundamental discovery reveals how such a diet could slow the aging process and may one day allow scientists to better treat or prevent age-related diseases, including heart disease, Alzheimer’s disease and many forms of cancer.
As the aging population continues to grow, age-related illnesses have become increasingly common. Already in the United States, nearly one in six people are over the age of 65. Heart disease continues to be the nation’s number one killer, with cancer and Alzheimer’s close behind. Such diseases place tremendous strain on patients, families and our healthcare system. But today, researchers in the laboratory of Gladstone Senior Investigator Eric Verdin, MD, have identified the role that a chemical compound in the human body plays in the aging process—and which may be key to new therapies for treating or preventing a variety of age-related diseases.
In the latest issue of the journal Science, available online today, Dr. Verdin and his team examined the role of the compound β-hydroxybutyrate (βOHB), a so-called “ketone body” that is produced during a prolonged low-calorie or ketogenic diet. While ketone bodies such as βOHB can be toxic when present at very high concentrations in people with diseases such as Type I diabetes, Dr. Verdin and colleagues found that at lower concentrations, βOHB helps protect cells from “oxidative stress”—which occurs as certain molecules build to toxic levels in the body and contributes to the aging process.
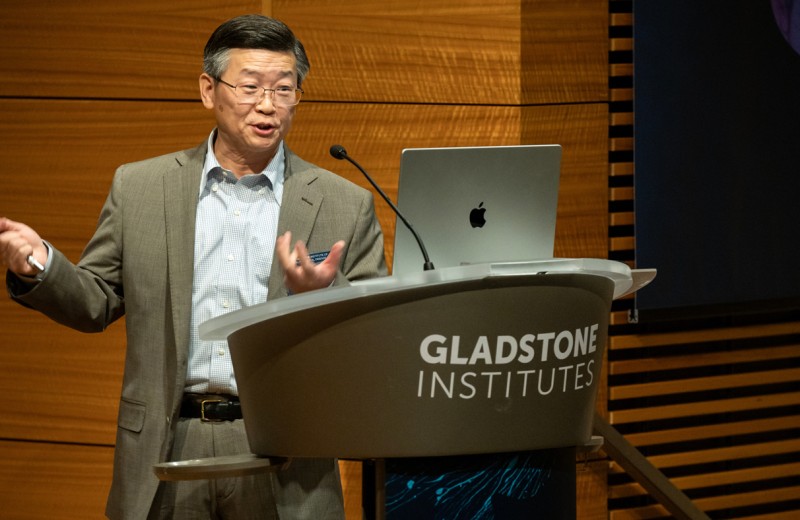
“Over the years, studies have found that restricting calories slows aging and increases longevity—however the mechanism of this effect has remained elusive” Dr. Verdin said. Dr. Verdin, the paper’s senior author, directs the Center for HIV & Aging at Gladstone and is also a professor at the University of California, San Francisco, with which Gladstone is affiliated. “Here, we find that βOHB—the body’s major source of energy during exercise or fasting—blocks a class of enzymes that would otherwise promote oxidative stress, thus protecting cells from aging.”
Oxidative stress occurs as cells use oxygen to produce energy, but this activity also releases other potentially toxic molecules, known as free radicals. As cells age, they become less effective in clearing these free radicals—leading to cell damage, oxidative stress and the effects of aging.
However, Dr. Verdin and his team found that βOHB might actually help delay this process. In a series of laboratory experiments—first in human cells in a dish and then in tissues taken from mice—the team monitored the biochemical changes that occur when βOHB is administered during a chronic calorie-restricted diet. The researchers found that calorie restriction spurs βOHB production, which blocked the activity of a class of enzymes called histone deacetylases, or HDACs.
Normally HDACs keep a pair of genes, called Foxo3a and Mt2, switched off. But increased levels of βOHB block the HDACs from doing so, which by default activates the two genes. Once activated, these genes kick-start a process that helps cells resist oxidative stress. This discovery not only identifies a novel signaling role for βOHB, but it could also represent a way to slow the detrimental effects of aging in all cells of the body.
“This breakthrough also greatly advances our understanding of the underlying mechanism behind HDACs, which had already been known to be involved in aging and neurological disease,” said Gladstone Investigator Katerina Akassoglou, PhD, an expert in neurological diseases and one of the paper’s co-authors. “The findings could be relevant for a wide range of neurological conditions, such as Alzheimer’s, Parkinson’s, autism and traumatic brain injury—diseases that afflict millions and for which there are few treatment options.”
“Identifying βOHB as a link between caloric restriction and protection from oxidative stress opens up a variety of new avenues to researchers for combating disease,” said Tadahiro Shimazu, a Gladstone postdoctoral fellow and the paper’s lead author. “In the future, we will continue to explore the role of βOHB—especially how it affects the body’s other organs, such as the heart or brain—to confirm whether the compound’s protective effects can be applied throughout the body.”
Matthew Hirschey, PhD, John Newman, MD, PhD, Wenjuan He, PhD, Kotaro Shirakawa, PhD, Natacha Le Moan, PhD, Carrie Grueter, PhD, Hyungwook Lim, PhD, Laura Saunders, PhD, and Robert V. Farese, Jr., MD, also participated in this research at Gladstone. This research was supported by the Gladstone Institutes.
Gladstone Presents Inaugural Sobrato Prize in Neuroscience to Yadong Huang, a Pioneer of Alzheimer’s Research
Gladstone Presents Inaugural Sobrato Prize in Neuroscience to Yadong Huang, a Pioneer of Alzheimer’s Research
The prize will be awarded annually to a Gladstone scientist who has made breakthrough discoveries in brain research; funds will help advance scientific discoveries from the lab to the clinic.
Awards News Release Alzheimer’s Disease Neurological Disease Huang Lab Aging Human GeneticsHope for Alzheimer’s: A Conversation with Gladstone’s Lennart Mucke
Hope for Alzheimer’s: A Conversation with Gladstone’s Lennart Mucke
Mucke, director of the Gladstone Institute of Neurological Disease, discusses what's next for Alzheimer’s research, the role of nonprofit research in developing new therapies, and why he's more hopeful than ever for a future where neurodegenerative diseases are fully treatable—and even preventable.
Alzheimer’s Disease Neurological Disease Mucke Lab AgingRyan Corces Joins Gladstone Institutes
Ryan Corces Joins Gladstone Institutes
A new lab to study the impact of lived experiences on developing Alzheimer’s disease
Institutional News News Release Profile Alzheimer’s Disease Data Science and Biotechnology Neurological Disease Corces Lab Aging