Gladstone NOW: The Campaign Join Us on the Journey✕
Gladstone researchers talk about the power of iPS cells in biomedical research, 15 years after Shinya Yamanaka first converted human skin cells into iPS cells.
In November 2007, Shinya Yamanaka, MD, PhD, senior investigator at Gladstone Institutes, demonstrated for the first time that he could “reprogram” human skin cells into cells that function like embryonic stem cells, meaning they can multiply indefinitely and transform into any cell type in the body. These reprogrammed cells are known as induced pluripotent stem cells, or iPS cells.
Yamanaka was awarded the 2012 Nobel Prize in Physiology or Medicine for this breakthrough. His discovery fundamentally changed biomedical research and opened up promising avenues for studying and treating unsolved diseases.
Fifteen years later, researchers at Gladstone—and all around the world—continue to use iPS cells to study the cause of disease, test potential drugs, and develop new treatment options. Four scientists explain the power of iPS cells in research.

Zoe Grant
Postdoctoral Scholar, Bruneau Lab
In the lab, I’m investigating the underlying causes of congenital heart defects, which are a group of heart diseases that affect roughly 1 in 100 live births. I’m using iPS cells, which I can turn into heart cells that beat in the dish—this is so incredible to watch.
I’m using iPS cells, which I can turn into heart cells that beat in the dish—this is so incredible to watch.
This has also revolutionized the way that I can do my research because I can work on human cells that haven’t come from rare patient samples, I can make and correct mutations, and I can generate the enormous number of cells that I need to understand the molecular mechanisms that underlie congenital heart defects.

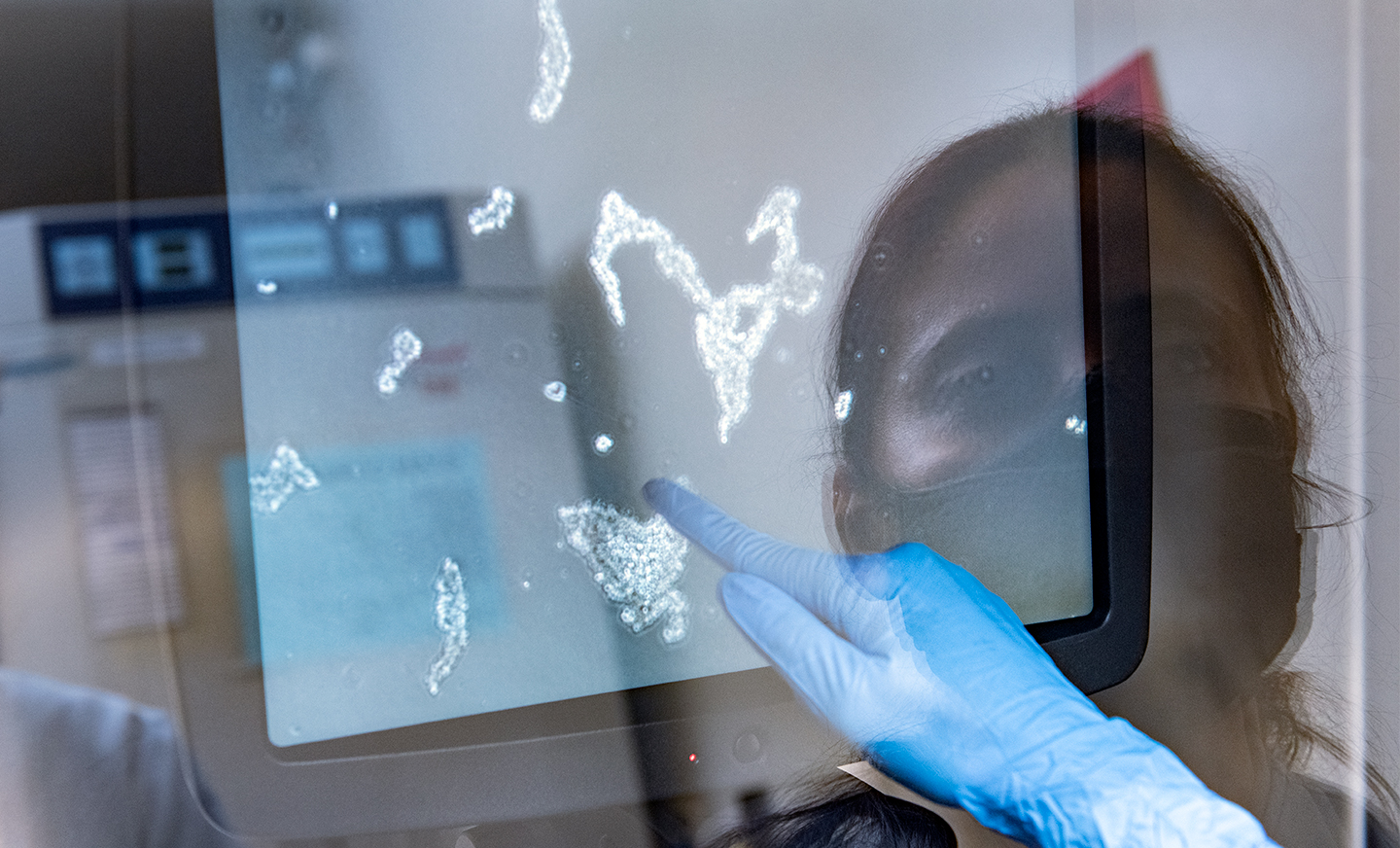
Ritu Kumar
Director, Stem Cell Core
The groundbreaking invention of induced pluripotent stem cells by Shinya Yamanaka not only gave hope to patients suffering from incurable diseases, but also laid a foundation for scientists to find treatments for the diseases that were considered untreatable before iPS cells.
IPS cells have given direction, acceleration, and meaning to my work in this new era of medical research.
The remarkable thing about this technology is that we collect only 1–5 milliliters of blood from patients, and we reprogram these blood cells to iPS cells, and then generate an unlimited number of mature, somatic cells (such as heart cells or brain cells) for disease modeling and drug discovery in a dish. IPS cells have given direction, acceleration, and meaning to my work in this new era of medical research.

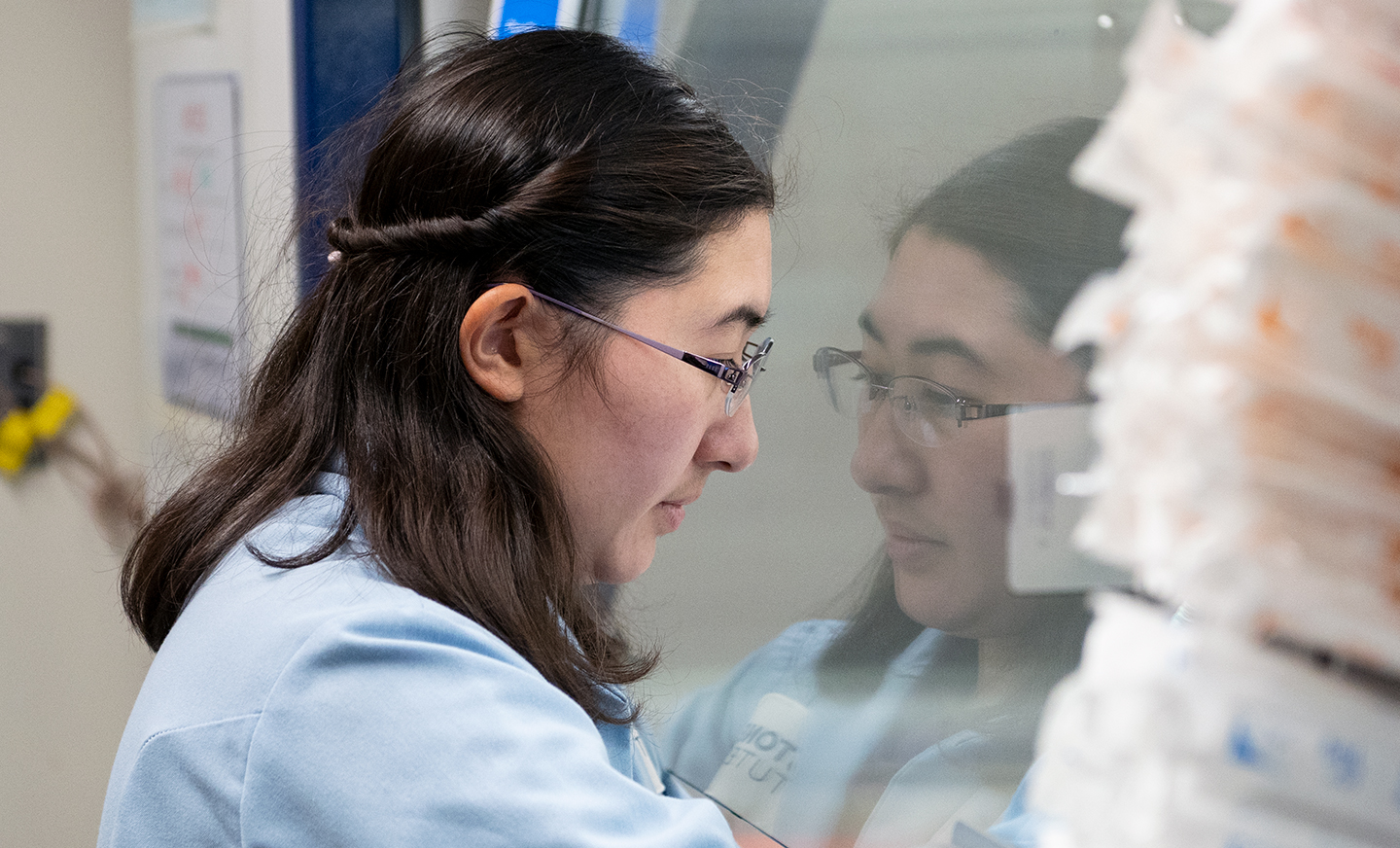
Wendy Runyon
Research Scientist, Stem Cell Core
I think one of the often overlooked benefits of iPS cells is the number of animal lives they save. Rodents and other animals have long been used as model systems, and I feel like many people forget about the debt we owe to research animals.
Using iPS cells can significantly reduce the number of animals that give their lives to scientific progress.
So many scientific breakthroughs have come from using animal model systems, and while I recognize their importance in research, using iPS cells can significantly reduce the number of animals that give their lives to scientific progress.
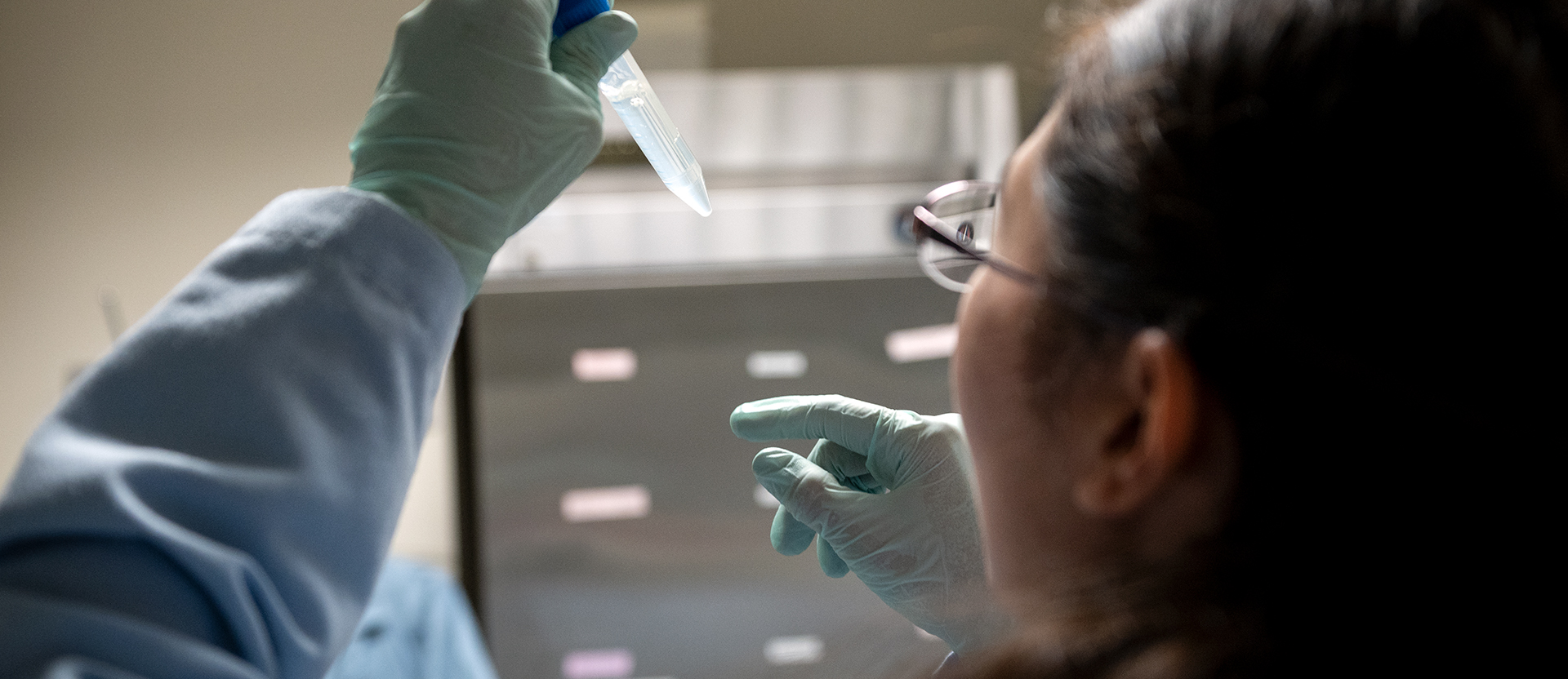

Ivana Vasic
Graduate Student, Yamanaka Lab
IPS cells are very cool, because they can generate any cell type that’s found in the body. However, one specific cell type that’s remained elusive is the human oocyte, or the egg.
IPS cells are very cool, because they can generate any cell type that’s found in the body.
My research focuses on using iPS cells to generate a very special type of cell, called a primordial germ cell. These cells are the direct stem cell precursors of oocytes. So if we can unlock this final step and actually mature primordial germ cells into oocytes, we could treat infertility and use these iPS cell–derived oocytes for in vitro fertilization.

A Sculptor of Modern Regenerative Medicine
A Sculptor of Modern Regenerative Medicine
Among his myriad accomplishments, Rudolf Jaenisch—winner of the 2025 Ogawa-Yamanaka Stem Cell Prize—was the first to demonstrate the potential of induced pluripotent stem cells to treat disease.
Awards Ogawa Stem Cell Prize Profile Regenerative Medicine Stem Cells/iPSCsDeepak Srivastava Selected to Deliver American Heart Association’s Distinguished Scientist Lecture
Deepak Srivastava Selected to Deliver American Heart Association’s Distinguished Scientist Lecture
Srivastava will present at the American Heart Association’s Scientific Sessions 2025 in New Orleans; the lectureship is a major recognition of excellence by the association.
News Release Cardiovascular Disease Srivastava Lab Genomics Stem Cells/iPSCsScience in Seconds | Researchers Pinpoint Key Gene Behind Heart Defects in Down Syndrome
Science in Seconds | Researchers Pinpoint Key Gene Behind Heart Defects in Down Syndrome
In this video, Gladstone scientists share how they used stem cells, gene editing, and AI to identify a gene driving heart defects in Down syndrome—and how reducing its levels in mice restored normal heart development, offering hope for future treatments
Gladstone Experts Cardiovascular Disease Data Science and Biotechnology Pollard Lab Srivastava Lab AI Big Data CRISPR/Gene Editing Human Genetics Stem Cells/iPSCs



