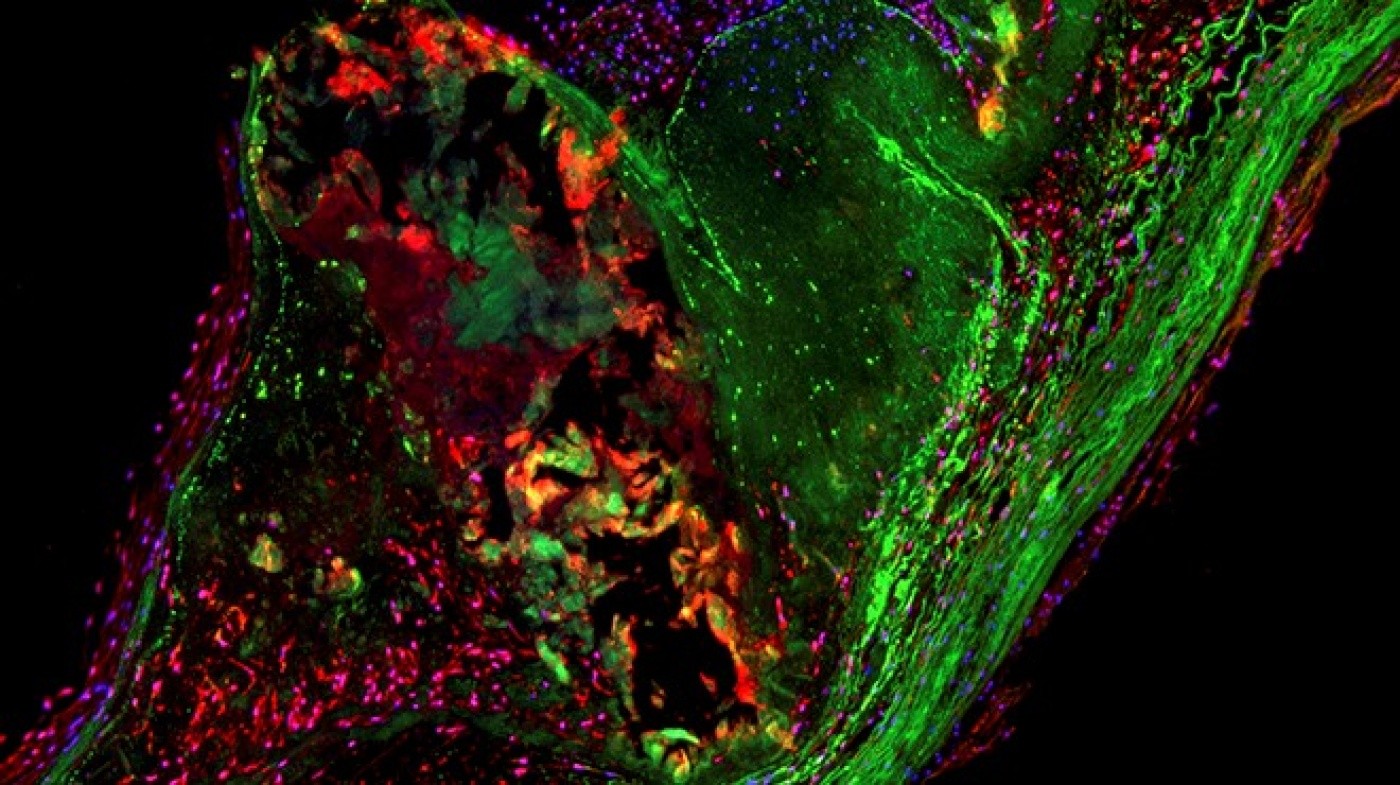
Gladstone scientists have identified the chain of events that causes healthy heart valves to harden like bone—and a potential way to correct this process by activating just a handful of genes. Their findings have tremendous implications for calcific aortic valve disease (CAVD), the third most common heart condition, and related forms of heart disease. [Image: Christina Theodoris]
Researchers from the Gladstone Institutes have used human cells to discover how blood flow in the heart protects against the hardening of valves in cardiovascular disease. What’s more, they’ve identified a potential way to correct this process when it goes wrong by flipping the switch on just a handful of genes. These findings may have implications for related conditions, like hardening of the arteries, which causes heart attacks and stroke.
Calcific aortic valve disease (CAVD) is the third leading cause of heart disease, affecting nearly 1.5 million people and resulting in 100,000 heart valve replacement surgeries in the U.S. alone. In CAVD, which can develop with age, heart valves begin to produce calcium, causing them to harden like bone. Scientists have long known that blood flow in the heart plays a role in the calcification of valves and arteries, but they did not understand how.
In a new study published in the journal Cell, Gladstone investigators reveal the chain of events that causes healthy valves to become bone-like. Senior author on the paper, Deepak Srivastava, MD, director of cardiovascular and stem cell research at Gladstone and a pediatric cardiologist at the University of California San Francisco (UCSF), had previously discovered that disruption of one of two copies of a master gene called NOTCH1 can cause valve birth defects and CAVD. In the current study, the researchers report that NOTCH1 acts like a sensor on the endothelial cells—the cells that line the valve and vessels—detecting blood flow outside of the cell and transmitting information to a network of genes inside the cell. Activation of NOTCH1 by blood flow causes a domino effect, triggering numerous other genes in the network to turn on or off, resulting in suppression of inflammation and calcification. However, if this process is disrupted by a decrease in NOTCH1, the cells become confused and start to act like bone cells, laying down calcium and leading to a deadly hardening of the valve.
In a collaborative effort between the Gladstone laboratories of Benoit Bruneau, PhD, Katherine Pollard, PhD, and Dr. Srivastava, the scientists used stem cell technology to make large amounts of endothelial cells from patients with CAVD, comparing them to healthy cells and mapping their genetic and epigenetic changes as they developed into valve cells. The researchers used the power of gene sequencing and clever computational methods to uncover the “source code” for human endothelial cells and learn how that code is disturbed in human disease.
“By understanding the gene networks that get disrupted in CAVD, we can pinpoint what we need to fix and find new therapeutics to correct the disease process,” says first author Christina Theodoris, an MD/PhD student at the Gladstone Institutes and UCSF.
Sifting through this mountain of data, the scientists found three key genes that were altered by the NOTCH1 mutation and also acted as master regulators, turning off the critical pathways that normally prevent inflammation and calcification. Remarkably, when the researchers manipulated the activity of these three genes, almost all of the other genes in the network were corrected, pointing to novel therapeutic targets for CAVD. The scientists are now screening for drugs that restore the gene network to its normal state.
“Identifying these master regulators is a big step in treating CAVD, not just in people with the NOTCH1 mutation, but also in other patients who experience calcification in their valves and arteries,” says Dr. Srivastava. “Now that we know how calcification happens and what the key nodes are, we know what genes to look for that might be mutated in other related forms of cardiovascular disease.”
Gladstone Team Uncovers Why Maternal Diabetes Predisposes Babies to Heart Defects
Gladstone Team Uncovers Why Maternal Diabetes Predisposes Babies to Heart Defects
The cutting-edge research methods that led to the discovery could be used to find other connections between environmental factors and birth defects.
News Release Research (Publication) Cardiovascular Disease Srivastava LabAmerican Heart Association Honors Gladstone President Deepak Srivastava with Distinguished Scientist Award
American Heart Association Honors Gladstone President Deepak Srivastava with Distinguished Scientist Award
The award recognizes leaders who have made major contributions to the fields of cardiovascular and stroke science
Awards News Release Cardiovascular Disease Srivastava LabWhen Two Disruptive Technologies Converge
When Two Disruptive Technologies Converge
How gene editing and stem cells are working in tandem at Gladstone Institutes to change science and medicine
Deep Dive Stem Cells/iPSCs CRISPR/Gene Editing Srivastava Lab Yamanaka Lab Doudna Lab Conklin Lab Marson Lab Huang Lab Ott Lab